How Compassion Meditation Rewires Your Brain & Cuts Inflammation

TL;DR: CMA is a selective cellular cleanup system that targets damaged proteins for degradation. As we age, CMA declines—leading to toxic protein accumulation and neurodegeneration. Scientists are developing therapies to restore CMA function and potentially prevent brain diseases.
Inside every one of your cells right now, a microscopic drama is playing out. Damaged proteins—twisted, misfolded, potentially toxic—are being identified, grabbed, and hauled away for destruction. This isn't the work of some general garbage collection system sweeping up everything in sight. It's chaperone-mediated autophagy (CMA), a remarkably selective cleanup mechanism that targets specific proteins for degradation. And when it stops working properly, the consequences can be devastating: Alzheimer's, Parkinson's, Huntington's disease.

The science behind CMA reveals why age is the single greatest risk factor for neurodegeneration. As we get older, this precision system starts to fail—not all at once, but gradually, relentlessly. Proteins that should be eliminated begin to accumulate. Cellular stress builds. And eventually, neurons start to die.
But here's what makes this moment different: researchers now understand CMA well enough to potentially restore its function. The question is whether we can turn that knowledge into therapies before too much damage is done.
Your cells have multiple garbage disposal systems. Macroautophagy works like a demolition crew, engulfing whole sections of cellular machinery in membrane bubbles and breaking them down. The proteasome system chews through tagged proteins like a wood chipper. Both are essential, both are powerful, and both are indiscriminate.
CMA is different. It doesn't bulk-degrade. It selects individual proteins based on a molecular signature—a specific pentapeptide motif related to KFERQ—embedded in their amino acid sequence. Roughly 30% of all cytosolic proteins carry this recognition sequence, making them potential CMA substrates. When a protein bearing this motif becomes damaged, oxidized, or otherwise problematic, CMA springs into action.
About 30% of all proteins in your cells carry the molecular signature that makes them potential targets for CMA. This precision targeting is what sets CMA apart from other cellular cleanup systems.
The process is elegant. A chaperone protein called HSC70 acts as the recognition agent, binding to the KFERQ-like motif on damaged proteins. HSC70 then escorts its cargo to the lysosome—the cell's digestive organelle—where it docks with a receptor called LAMP-2A. Think of LAMP-2A as the lysosomal gatekeeper. When a substrate protein binds to LAMP-2A, the receptor oligomerizes, forming a channel through which the unfolded protein can slide into the lysosome's acidic interior. Once inside, digestive enzymes reduce the protein to amino acids that can be recycled.
This isn't just housekeeping. CMA plays critical roles in cellular metabolism, stress response, and immune function. It degrades lipid droplet proteins like perilipin 2 and 3, controlling fat metabolism. During prolonged starvation—after about ten hours—cells switch from macroautophagy to CMA, because CMA is more selective and energy-efficient.
Most importantly for neurodegeneration, CMA specifically targets the proteins that go wrong in brain diseases.
Understanding how CMA works requires looking at the molecular players in detail. The system hinges on three key components: the recognition chaperone, the lysosomal receptor, and the translocation complex.
HSC70, short for heat shock cognate protein 70, is the scout. Unlike its stress-induced cousin HSP70, HSC70 is constitutively expressed—always present, always vigilant. It patrols the cytosol looking for proteins displaying the KFERQ-like motif in an accessible configuration. The motif itself is a biochemically defined sequence: one lysine (K), one phenylalanine (F), one glutamic or aspartic acid (E), one arginine (R), and one glutamine (Q). The exact sequence varies, but the chemical properties must match. When HSC70 recognizes a substrate, it binds tightly, keeping the protein unfolded and preventing aggregation.

LAMP-2A, the lysosomal receptor, is where CMA's selectivity becomes physical exclusivity. LAMP-2A is one of three splice variants of the LAMP2 gene. While LAMP-2B and LAMP-2C have other roles, LAMP-2A is uniquely dedicated to CMA. It's a single-spanning membrane protein embedded in the lysosomal membrane, with its C-terminal tail facing the cytosol. That tail is what HSC70-bound substrates recognize and bind to.
Here's the crucial part: binding triggers multimerization. Individual LAMP-2A monomers assemble into a multimeric translocation complex—essentially a protein-conducting channel. The substrate protein must unfold completely to pass through. Once the protein enters the lysosomal lumen, a different chaperone, lysosomal HSC70, pulls it fully inside. The LAMP-2A complex then disassembles, recycling its components for the next round.
This dynamic assembly and disassembly is energy-intensive but allows exquisite control. The cell can regulate CMA activity simply by controlling how much LAMP-2A is present at the lysosomal membrane. More LAMP-2A means more translocation sites; less LAMP-2A means reduced CMA.
And that's exactly what happens when we age.
The proteins that define neurodegenerative diseases—alpha-synuclein in Parkinson's, tau in Alzheimer's, huntingtin in Huntington's—are all CMA substrates. They all contain KFERQ-like motifs. And under normal circumstances, CMA degrades them efficiently.
Take alpha-synuclein, the protein whose aggregation forms the Lewy bodies characteristic of Parkinson's disease. Wild-type alpha-synuclein contains a KFERQ-like motif—specifically, the sequence VKKDQ. Healthy CMA recognizes and degrades it continuously, preventing accumulation. Studies show that overexpressing LAMP-2A in cellular and animal models of Parkinson's dramatically reduces alpha-synuclein burden and even rescues motor deficits.
"CMA specifically degrades physiologic alpha-synuclein, whereas pathologic alpha-synuclein inhibits CMA, thus enhancing aggregation of itself and other Lewy body components."
— Frontiers in Molecular Neuroscience
But pathological alpha-synuclein—the mutant or post-translationally modified forms that drive disease—behaves differently. These aberrant forms still bind to LAMP-2A, but they don't translocate properly. Instead, they clog the receptor, blocking degradation of other CMA substrates. It's a vicious cycle: damaged alpha-synuclein inhibits CMA, which allows more alpha-synuclein to accumulate, which further inhibits CMA. The result is a feed-forward loop of protein aggregation.
The same pattern appears in other neurodegenerative diseases. Mutant tau in tauopathies binds LAMP-2A with abnormal affinity, creating a similar clogging effect. Mutant huntingtin impairs CMA through multiple mechanisms. In each case, the disease protein doesn't just resist degradation—it actively sabotages the degradation system itself.

Genetic factors compound the problem. Mutations in genes like LRRK2 and VPS35, both associated with familial Parkinson's disease, reduce LAMP-2A trafficking to the lysosomal membrane. Fewer receptors means less CMA activity, even when HSC70 is working fine. The proteins pile up. Neuronal stress increases. And disease accelerates.
If there's one consistent finding across CMA research, it's this: CMA activity declines with age in almost every tissue studied. This has been demonstrated in rodent models and confirmed in cells from older humans. The decline is gradual but significant, and it tracks closely with the rising incidence of neurodegenerative disease.
The primary culprit is LAMP-2A. As animals age, LAMP-2A levels at the lysosomal membrane drop. Importantly, this isn't because cells stop making LAMP-2A—gene expression and protein synthesis rates remain relatively stable. The problem is receptor stability. LAMP-2A breaks down faster in aged cells. It's degraded more quickly, and the mechanisms that normally stabilize it at the membrane become less effective.
Several factors contribute. Lipid composition of lysosomal membranes changes with age, making them less hospitable to LAMP-2A. Oxidative stress damages the receptor directly. And the cellular machinery that regulates LAMP-2A levels—including the very chaperones that help fold and stabilize it—also decline.
HSC70 levels may drop too, though the evidence is mixed. Some studies show decreased HSC70 in aged brains, particularly in regions affected by neurodegeneration. Others find HSC70 relatively preserved. What's clear is that even if HSC70 remains abundant, a shortage of LAMP-2A creates a bottleneck that cripples CMA.
The age-related decline in CMA isn't caused by cells making less LAMP-2A. Instead, the receptor becomes unstable and breaks down faster—a critical distinction that points toward receptor stabilization as a therapeutic strategy.
There's an interesting twist: high-fat diets inhibit CMA by reducing LAMP-2A stability. This suggests lifestyle factors could accelerate age-related CMA decline. Conversely, interventions like exercise appear to support autophagic function generally, though specific effects on CMA are still being mapped.
The implications are stark. As CMA weakens, damaged proteins linger longer. Cellular stress mounts. And the proteins most likely to cause problems—those prone to misfolding and aggregation—are precisely the ones CMA is supposed to eliminate. It's a setup for neurodegeneration.
Impaired CMA doesn't just mean slower protein turnover. It triggers cascading cellular dysfunction that amplifies disease risk.
First, there's direct protein accumulation. When CMA can't degrade alpha-synuclein, tau, or huntingtin efficiently, these proteins build up in the cytosol. Elevated concentrations increase the likelihood of misfolding and aggregation. Oligomers form—toxic intermediate species that disrupt cellular membranes, interfere with synaptic function, and seed further aggregation.
Second, CMA dysfunction overloads compensatory pathways. Macroautophagy and the proteasome can partially compensate for lost CMA activity, but they're not perfect substitutes. Macroautophagy is less selective, consuming valuable cellular components along with damaged proteins. The proteasome is better at degrading individual proteins but struggles with aggregates. When both systems are chronically stressed, cellular homeostasis—proteostasis—collapses.

Third, metabolic consequences ripple outward. CMA regulates lipid metabolism by degrading perilipin proteins that coat lipid droplets. Without functional CMA, lipid droplets accumulate, disrupting energy metabolism and contributing to cellular stress. This may explain why metabolic dysfunction and neurodegeneration so often coincide.
Fourth, the immune system gets involved. Protein aggregates activate inflammatory pathways. Microglia—the brain's immune cells—respond to accumulating debris, releasing inflammatory cytokines. In the short term, this helps clear damage. Chronically, it drives neuroinflammation, which accelerates neuronal death.
The endpoint is a vicious cycle. Reduced CMA leads to protein accumulation, which causes cellular stress, which further impairs CMA, which leads to more accumulation. Breaking this cycle is the goal of therapeutic intervention.
The good news: scientists have identified multiple ways to potentially restore or enhance CMA function. The challenge is translating laboratory findings into safe, effective treatments for humans.
Direct LAMP-2A upregulation is the most straightforward approach. If declining LAMP-2A is the bottleneck, boost its levels. Gene therapy experiments overexpressing LAMP-2A in mouse models of Parkinson's disease have shown dramatic benefits: reduced alpha-synuclein pathology, preserved dopaminergic neurons, and improved motor function. In some models, the effects were essentially curative.
Transgenic mice engineered to maintain normal LAMP-2A levels throughout life show improved stress response and healthspan. They handle cellular stressors better and age more slowly, at least by some metrics. This validates LAMP-2A as a therapeutic target but doesn't solve the delivery problem. Getting genes into adult human brains safely and efficiently remains difficult.
"Overexpression of LAMP-2A efficiently prevents alpha-synuclein burden in cellular and animal models of Parkinson's disease and counteracts motor deficits."
— Frontiers in Molecular Neuroscience
Small molecule activators offer a more practical route. Researchers have identified retinoic acid derivatives that activate CMA in cultured cells. These compounds appear to increase LAMP-2A stability or expression, though the exact mechanisms are still being worked out. Other candidates modulate upstream signaling pathways—like mTOR inhibition or NRF2 activation—that influence autophagic activity broadly.
One clever strategy targets both CMA and macroautophagy simultaneously. Because the two pathways compensate for each other, boosting both together produces synergistic neuroprotection. Drugs that upregulate multiple autophagy pathways might be more effective than CMA-specific interventions.
Lipid modulation is another angle. Since membrane lipid composition affects LAMP-2A stability, dietary interventions or drugs that normalize lysosomal membranes could indirectly support CMA. This is speculative but aligns with observations that metabolic health influences neurodegeneration risk.

Exercise and lifestyle interventions aren't specific to CMA but support autophagic function generally. Physical activity upregulates autophagy-related genes, improves mitochondrial function, and reduces oxidative stress—all factors that likely help maintain CMA. While exercise won't cure Parkinson's or Alzheimer's, it might slow disease progression by supporting cellular quality control systems.
Here's the hard truth: no clinical trial targeting CMA has yet succeeded in treating neurodegenerative disease. We have compelling preclinical data—animal studies showing robust effects—but translating those findings to human patients has proven difficult.
Part of the problem is timing. By the time someone is diagnosed with Parkinson's or Alzheimer's, substantial neuronal loss has already occurred. Restoring CMA at that stage might slow progression but won't reverse damage. Preventive strategies—boosting CMA before symptoms appear—would be more effective but require identifying at-risk individuals early, which we can't yet do reliably.
Another issue is measurement. We lack good biomarkers for CMA activity in living humans. Cerebrospinal fluid levels of LAMP-2 change little with age, making them poor indicators. We can't easily biopsy brain tissue to measure LAMP-2A directly. This makes it hard to know whether CMA-targeting drugs are actually working in patients, even if we can see effects in lab models.
One of the biggest obstacles to developing CMA therapies is that we can't easily measure whether treatments are working in living patients. Better biomarkers are urgently needed.
Delivery is another challenge. Getting therapeutic molecules across the blood-brain barrier is notoriously difficult. Gene therapies require invasive administration. Small molecules must be brain-penetrant, which limits chemical options. And CMA operates inside lysosomes, adding another membrane barrier.
Then there's safety. Cranking up autophagy sounds good, but autophagy also degrades functional proteins and organelles. Excessive activation could cause cellular starvation or disrupt normal metabolism. Finding the therapeutic window—enough CMA upregulation to clear pathological proteins without harming healthy cellular processes—will require careful dose-finding studies.
Despite these obstacles, interest is growing. Drug development programs are exploring autophagy modulators for neurodegenerative diseases. Some target macroautophagy, others aim at lysosomal function broadly, and a few are specifically investigating CMA. We're still in early phases, but the foundation is being laid.
Moving forward, several research priorities stand out.
Better biomarkers are essential. We need ways to measure CMA activity in living people—ideally through blood tests or brain imaging. New fluorescent reporters that track CMA flux are being developed for research use. Adapting these for clinical diagnostics would be transformative.
Understanding CMA regulation more deeply will reveal new intervention points. We know LAMP-2A levels matter, but what controls its stability? Are there post-translational modifications that could be targeted? How do other proteins regulate LAMP-2A trafficking? Answering these questions could identify novel drug targets.
Combination therapies may prove more effective than single-pathway approaches. Since CMA, macroautophagy, and the proteasome work together to maintain proteostasis, therapies that support all three might outperform CMA-only interventions. Adding anti-inflammatory or mitochondrial-protective agents could further enhance benefits.
Personalized medicine will matter. Not all neurodegenerative diseases impair CMA the same way. Genetic background, disease stage, and comorbidities all influence how CMA dysfunction manifests. Tailoring interventions to individual patients—boosting LAMP-2A in one case, stabilizing membranes in another—could improve outcomes.
Exploring CMA beyond the brain might uncover unexpected applications. CMA dysfunction contributes to liver disease, metabolic disorders, and possibly cancer. Therapeutic strategies developed for neurodegeneration could benefit other conditions, and vice versa. Cross-pollination between disease areas often accelerates progress.
Finally, there's the question of prevention. If we can identify people at high risk for CMA decline—through genetics, lifestyle factors, or early biomarkers—we might intervene before irreversible damage occurs. This is speculative, but the same approach has worked for cardiovascular disease and diabetes. Why not neurodegeneration?
Chaperone-mediated autophagy sits at the intersection of aging and disease. It's a fundamental cellular quality control system that keeps neurons healthy, and its failure is a major driver of neurodegeneration. We now understand its molecular machinery well enough to envision therapeutic interventions.
The challenge is execution. Turning knowledge into treatments requires solving problems of drug delivery, biomarker development, clinical trial design, and safety. It requires sustained funding, collaboration across disciplines, and willingness to fail and iterate. Most of all, it requires time—something patients with Alzheimer's or Parkinson's don't have in abundance.
But the opportunity is real. If we can restore CMA function in aging brains, we might prevent or slow the diseases that rob people of their memories, their mobility, their independence. We might extend not just lifespan but healthspan, keeping neurons functional into old age.
This isn't science fiction. The basic biology is understood. Animal models work. The pieces are in place. Now comes the hard part: making it work in humans.
The next decade will tell us whether CMA-targeted therapies join the arsenal against neurodegeneration—or remain a promising idea that didn't pan out. Either way, CMA research has already reshaped how we think about aging, protein homeostasis, and brain health. It's shown us that cellular garbage disposal isn't boring housekeeping; it's a matter of life and death for neurons.
And it's given us a specific target to aim at. In a field often characterized by frustration and failure, that's progress worth celebrating.
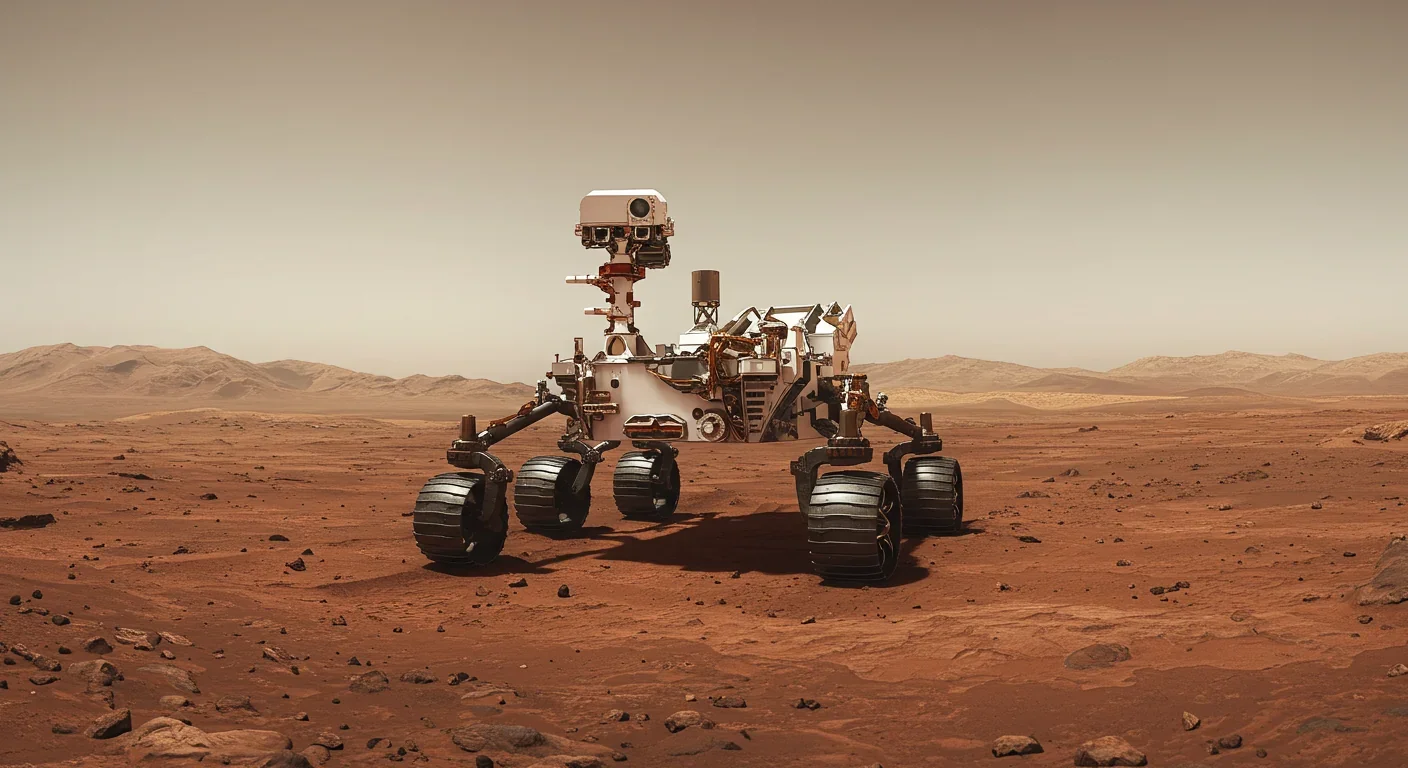
Curiosity rover detects mysterious methane spikes on Mars that vanish within hours, defying atmospheric models. Scientists debate whether the source is hidden microbial life or geological processes, while new research reveals UV-activated dust rapidly destroys the gas.

CMA is a selective cellular cleanup system that targets damaged proteins for degradation. As we age, CMA declines—leading to toxic protein accumulation and neurodegeneration. Scientists are developing therapies to restore CMA function and potentially prevent brain diseases.

Intercropping boosts farm yields by 20-50% by growing multiple crops together, using complementary resource use, nitrogen fixation, and pest suppression to build resilience against climate shocks while reducing costs.

The Baader-Meinhof phenomenon explains why newly learned information suddenly seems everywhere. This frequency illusion results from selective attention and confirmation bias—adaptive evolutionary mechanisms now amplified by social media algorithms.

Plants and soil microbes form powerful partnerships that can clean contaminated soil at a fraction of traditional costs. These phytoremediation networks use biological processes to extract, degrade, or stabilize toxic pollutants, offering a sustainable alternative to excavation for brownfields and agricultural land.

Renters pay mortgage-equivalent amounts but build zero wealth, creating a 40x wealth gap with homeowners. Institutional investors have transformed housing into a wealth extraction mechanism where working families transfer $720,000+ over 30 years while property owners accumulate equity and generational wealth.
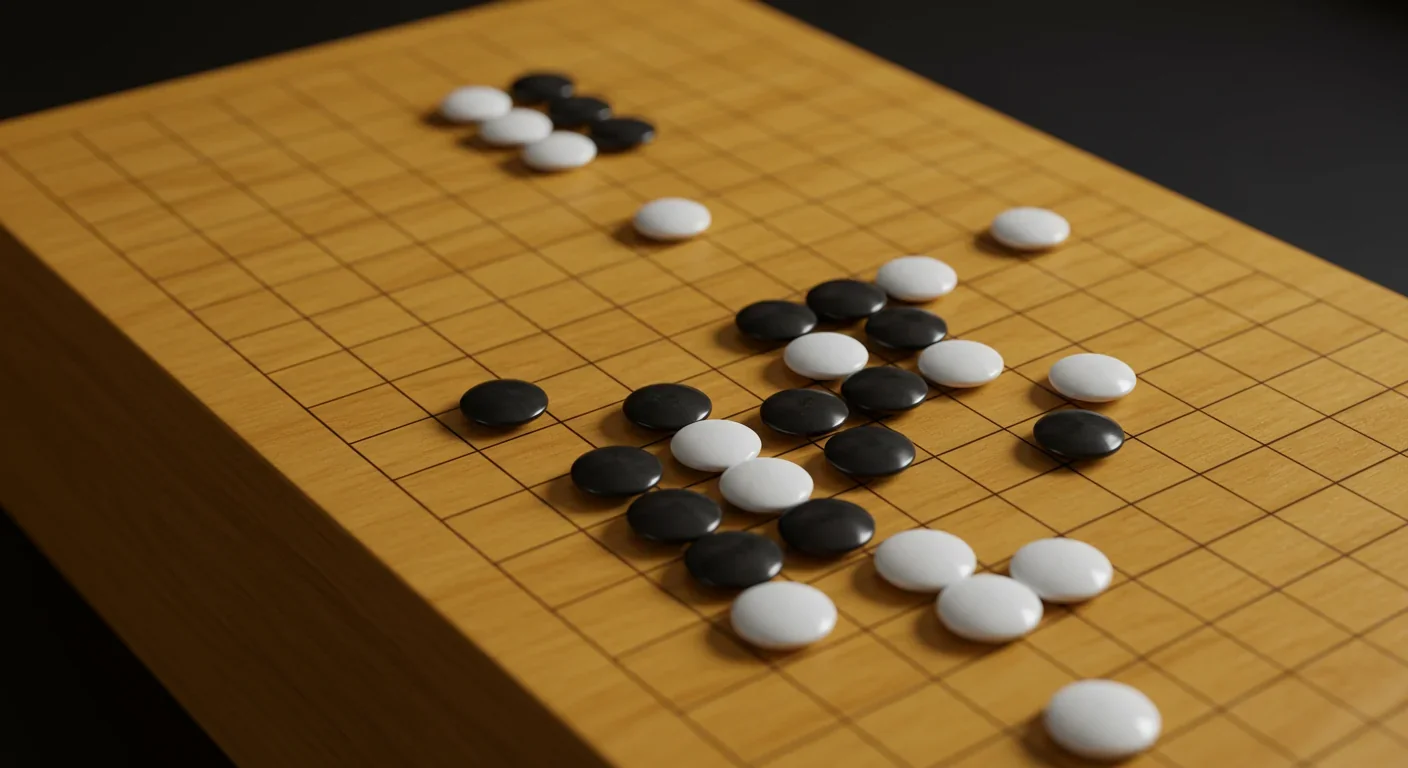
AlphaGo revolutionized AI by defeating world champion Lee Sedol through reinforcement learning and neural networks. Its successor, AlphaGo Zero, learned purely through self-play, discovering strategies superior to millennia of human knowledge—opening new frontiers in AI applications across healthcare, robotics, and optimization.