Your Cell's Protein Cleanup Fails With Age—Causing Brain Disease

TL;DR: Cross-link breakers are experimental drugs that could reverse arterial stiffening by breaking down AGE cross-links in blood vessel walls. Early compounds like alagebrium showed promise in animals but failed in humans because they didn't target glucosepane, the dominant cross-link in human tissue. New research funded by SENS Foundation is developing glucosepane-specific breakers that could genuinely reverse vascular aging.
Imagine waking up one day to find your arteries are as flexible as they were decades ago. That's not science fiction anymore—researchers are closing in on a class of compounds called cross-link breakers that could reverse the molecular damage causing your blood vessels to stiffen with age. Unlike today's heart medications that merely manage symptoms, these drugs aim to undo the underlying structural damage, potentially transforming how we treat cardiovascular disease in aging populations.
Your arteries are supposed to expand and contract with every heartbeat, absorbing the pressure surge and delivering smooth, steady blood flow to your organs. But as you age, something sinister happens at the molecular level. Proteins in your arterial walls become glued together by chemical bonds called advanced glycation end-products (AGEs), turning supple vessels into rigid pipes. This stiffening drives up blood pressure, strains your heart, and sets the stage for heart failure, stroke, and cognitive decline.
Most people have never heard of arterial stiffness, yet it's one of the most reliable predictors of cardiovascular death. When scientists measure pulse wave velocity—how fast pressure waves travel through your arteries—they find a grim correlation: each 1 meter per second increase in arterial stiffness raises your risk of cardiovascular events by 36%, cardiovascular death by 41%, and all-cause mortality by 37%.
The numbers get worse with age. In healthy people under 10, pulse waves move through arteries at about 5.4 meters per second. By age 60, that speed nearly doubles to 9.8 m/s. By 80, it hits 11 m/s. This isn't just a measurement quirk—it's your body literally turning to stone from the inside out.
Arterial stiffness measured by pulse wave velocity is so predictive that each 1 m/s increase raises cardiovascular death risk by 41%. Your arteries are aging faster than you think.
The culprit? A molecule called glucosepane, the most abundant cross-linking AGE in human tissue. Glucosepane forms when glucose in your blood reacts with proteins in your arterial walls through a process called the Maillard reaction—the same chemistry that browns bread when you toast it. But instead of creating a crispy crust, it creates covalent bonds between collagen fibers, welding them into an inflexible mesh.
Here's what makes glucosepane so insidious: it accumulates at levels 10 to 1,000 times higher than any other cross-linking AGE. In a 90-year-old's skin, glucosepane accounts for about 50 times the total protein cross-linking of all other types combined. Your arteries experience the same relentless accumulation, decade after decade, with no natural mechanism to break these bonds once they form.
For most of medical history, we've treated the consequences of stiff arteries—lowering blood pressure with drugs, implanting stents, performing bypass surgery. What we couldn't do was reverse the fundamental damage. That changed when researchers asked a simple question: if chemical bonds can form, why can't they be broken?
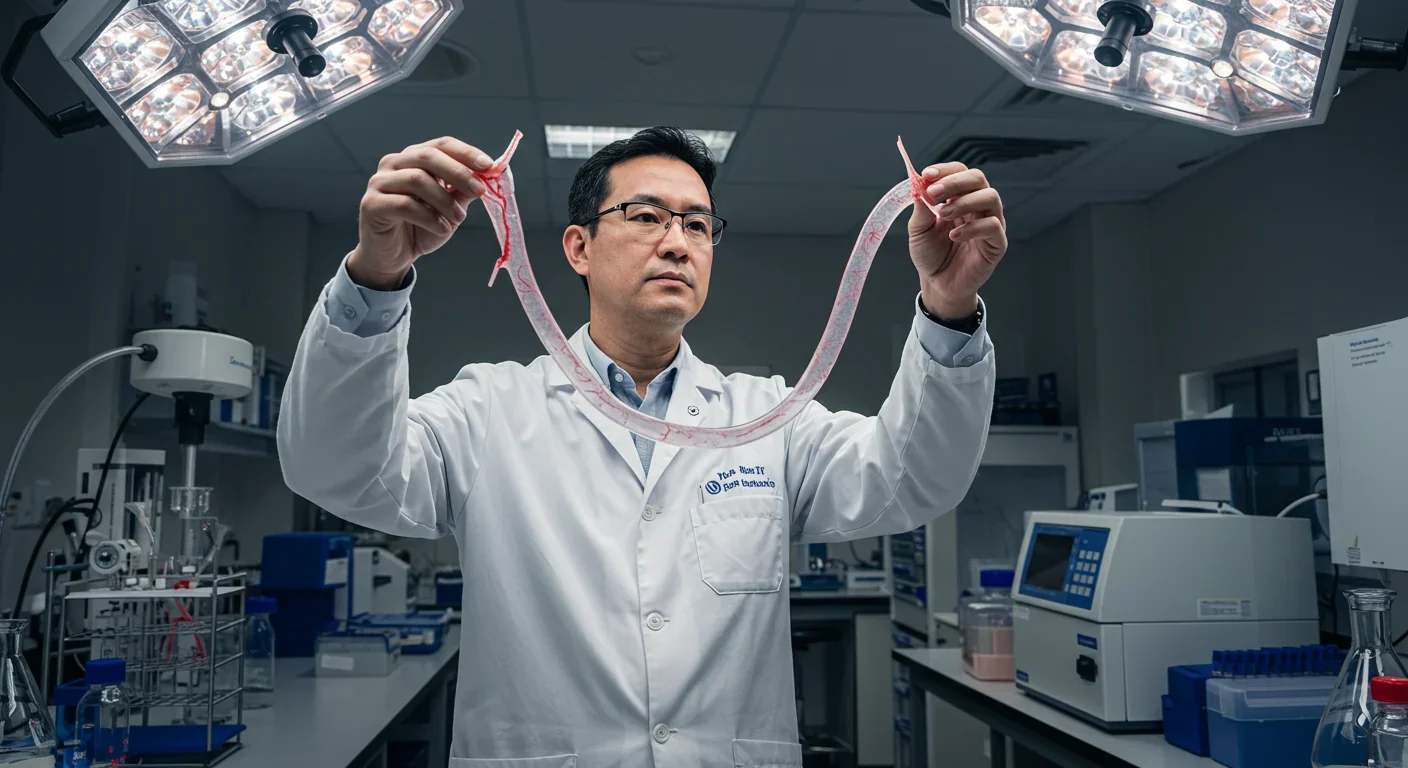
Cross-link breakers work by cleaving the carbon-carbon bonds within established AGE cross-links. Think of arterial collagen as a tangled fishing net where glucosepane acts like dozens of knots tying the fibers together. Cross-link breakers are molecular scissors that cut these knots, freeing the collagen fibers to move independently again.
The first compound to prove this concept was alagebrium (ALT-711), a thiazolium derivative developed in the early 2000s. Animal studies were spectacular. In rats, alagebrium reduced large artery stiffness, enhanced cardiac output, and improved the heart's ability to fill during the relaxation phase between beats. When researchers tested it in elderly humans with vascular stiffening, arterial compliance improved by approximately 15% after just 56 days. In some studies, carotid artery stiffness dropped by 37%.

But there was a problem, and it illustrates why translating animal research to humans is so tricky.
Alagebrium's development was discontinued in 2009, but not because of safety issues—the compound exhibited a favorable safety profile in human studies. The company simply ran out of money and couldn't secure a drug license. Yet even if funding had continued, there was a deeper scientific hurdle.
Rats and humans age differently at the molecular level. The AGE cross-links that accumulate in rat arteries aren't the same as those in human tissue. Alagebrium was fantastic at breaking the cross-links dominant in rats, but glucosepane is the overwhelming majority of AGEs in human tissue, and alagebrium didn't effectively target it.
"Alagebrium had no independent effect on vascular function, nor did it potentiate the effect of exercise training."
— Clinical trial researchers, as reported in LONGECITY forum
This explains why a one-year randomized trial in 48 older adults found no improvement in arterial stiffness with alagebrium treatment. The drug wasn't breaking the right bonds. It was like bringing bolt cutters to a padlock that requires a key.
The failure of alagebrium sent a clear message to researchers: if you want to reverse arterial aging in humans, you need to target glucosepane specifically. That's harder than it sounds. Glucosepane is chemically complex, and until recently, scientists couldn't even synthesize it in the lab to study potential breakers.
Today, the field is experiencing a renaissance thanks to breakthroughs in glucosepane chemistry. The SENS Research Foundation has funded research to produce the tools needed to work with glucosepane and demonstrate that it can be cleared from tissues. This work has opened the door to developing second-generation cross-link breakers that actually match the human aging process.
One promising approach uses α-dicarbonyl traps like aminoguanidine, which intercept the intermediate compounds that precede glucosepane formation. Instead of breaking existing cross-links, these compounds prevent new ones from forming in the first place. In rat studies, aminoguanidine reduced cross-link accumulation without interfering with normal aging processes.

Another strategy uses modified thiazolium salts—chemical cousins of alagebrium—engineered to attack glucosepane's specific chemical structure. These bidentate nucleophiles target the adjacent carbonyl groups in the α-dicarbonyl intermediate, cleaving the carbon-carbon bond before the final cross-link forms.
But the most exciting frontier is genuine glucosepane breakers: compounds that can dissolve existing cross-links in aging tissue. If successful, these drugs wouldn't just slow arterial stiffening—they'd reverse it, potentially restoring decades of lost vascular elasticity.
Arterial stiffness doesn't exist in isolation. Your cardiovascular system connects to every organ, and stiff arteries create cascading damage throughout your body.
When arteries lose elasticity, the heart works harder with every beat, leading to left ventricular hypertrophy—the heart muscle thickens and eventually weakens. Stiff arteries also alter the timing of reflected pressure waves. In healthy young vessels, these reflections arrive during the heart's relaxation phase, helping coronary arteries fill with blood. In stiff arteries, reflections return too early, during contraction, increasing the workload and reducing coronary perfusion.
In a 90-year-old, glucosepane causes 50 times more protein cross-linking than all other types combined. This single molecule may be the key to unlocking vascular rejuvenation.
Your brain pays a heavy price. The delicate capillaries in your brain evolved to receive steady, cushioned blood flow. When stiff arteries deliver pulsatile, high-pressure surges instead, it damages these fragile vessels, contributing to vascular dementia and cognitive decline. Studies consistently show that people with higher pulse wave velocity perform worse on memory tests and have higher rates of white matter lesions.
Your kidneys suffer too. Renal blood vessels face similar damage from unregulated pressure pulsations, accelerating chronic kidney disease in older adults and people with diabetes.
This is why targeting arterial cross-links matters so much. Breaking these bonds could simultaneously improve heart function, preserve cognitive ability, and protect kidney health—a single intervention with systemic anti-aging effects.
Cross-link breakers aren't the only game in town. A parallel revolution in vascular aging targets cellular senescence—the process where cells stop dividing and start secreting inflammatory molecules that damage surrounding tissue.

Senescent cells accumulate in aging arteries, where they adopt a pro-inflammatory secretory phenotype that accelerates stiffness. Drugs called senolytics selectively eliminate these zombie cells, and animal studies show remarkable results. In aged mice, senolytic treatment improved vascular compliance and reduced arterial stiffness.
Could combining senolytics with cross-link breakers produce even better results? It's an intriguing possibility. Senolytics would clear out the inflammatory cells driving ongoing damage, while cross-link breakers would undo existing structural harm. Together, they might achieve what neither can alone: comprehensive vascular rejuvenation.
"The laboratory studies were very compelling, we were able to make aging blood vessels behave as if they were young again."
— Dr. Tory Hagen, Oregon State University
There's also renewed interest in the ceramide-phosphatase axis. Researchers at Oregon State University discovered that ceramides—fatty molecules that accumulate in aging vessels—drive excessive phosphatase activity, which impairs the signaling needed for smooth muscle relaxation. When they inhibited ceramide synthesis in rat blood vessels, aging vessels behaved as if they were young again. This approach targets vascular function rather than structure, but it could complement cross-link breakers beautifully.
So when will these drugs reach patients? That's the question everyone wants answered, and the honest answer is: we don't know yet, but we're closer than ever before.
The scientific foundation is solid. We understand the biochemistry of glucosepane formation. We have tools to synthesize and study it. We've proved the concept in animals. What's missing is the translational work—finding the right compound, optimizing its structure for safety and efficacy, and conducting human trials.
Clinical trials for new drugs typically take 10 to 15 years from initial discovery to FDA approval, assuming everything goes well. Cross-link breakers face additional hurdles because they're targeting a novel mechanism. Regulators will need convincing that breaking protein cross-links is safe, that it doesn't compromise arterial integrity or create unforeseen problems.
One advantage: we have excellent biomarkers. Pulse wave velocity can be measured non-invasively using devices like the Arteriograph, providing objective evidence of whether a drug is working within weeks or months. That's much faster than waiting years to see if heart attacks decrease.

Another encouraging sign: the aging population creates enormous market incentives. Cardiovascular disease remains the leading cause of death globally, and conventional treatments don't address the root cause. A drug that genuinely reverses arterial aging could become one of the most prescribed medications in history.
While we wait for glucosepane breakers, you're not powerless. Lifestyle interventions can slow—though not reverse—arterial stiffening.
Exercise is the most potent tool available. Regular physical activity improves arterial flexibility and reduces pulse wave velocity, even in older adults. Aerobic exercise seems particularly effective, though resistance training helps too. The key is consistency—three to five sessions per week produce measurable benefits.
Diet matters. Diets high in added sugars accelerate AGE formation (remember, glucose is the starting ingredient for glucosepane). Reducing sugar intake and focusing on whole foods can slow the glycation process. Some evidence suggests that compounds in green tea, certain spices, and antioxidant-rich foods may inhibit AGE formation, though the effects are modest.
You can start protecting your arteries now: exercise 3-5 times weekly, reduce sugar intake, control blood pressure, and manage diabetes aggressively. These steps slow AGE accumulation while researchers work on drugs to reverse it.
Blood pressure control is crucial. Hypertension both results from and contributes to arterial stiffness in a vicious cycle. Managing blood pressure with medication when needed protects your arteries while we wait for better solutions.
And if you have diabetes, aggressive glucose control is essential. People with diabetes accumulate glucosepane much faster than non-diabetics, making them prime candidates for future cross-link breaker therapy.
Picture healthcare in 2040. A patient visits their doctor for a routine checkup at age 60 and learns their pulse wave velocity has crept into the high-risk range. Instead of simply starting blood pressure medication, the doctor prescribes a glucosepane breaker. Over six months, the patient's arterial stiffness drops to levels typical of someone 20 years younger. Their blood pressure normalizes without medication. Their brain receives steady, gentle blood flow again. The trajectory of their health—once aimed at heart failure and dementia—shifts dramatically.
That future isn't guaranteed, but it's plausible. The science is real, the targets are validated, and the need is undeniable. Every person over 50 is accumulating glucosepane right now, ticking toward cardiovascular disease one cross-link at a time.
The question isn't whether we can break those bonds—early research says we can. The question is whether we'll invest the resources to turn that laboratory possibility into a medicine millions can take. If we do, we won't just be treating a disease. We'll be attacking one of the fundamental processes of aging itself, potentially adding years of vitality to billions of lives.
The bonds that stiffen our arteries formed slowly, almost imperceptibly, over decades. Breaking them might just be the breakthrough that changes how we age.
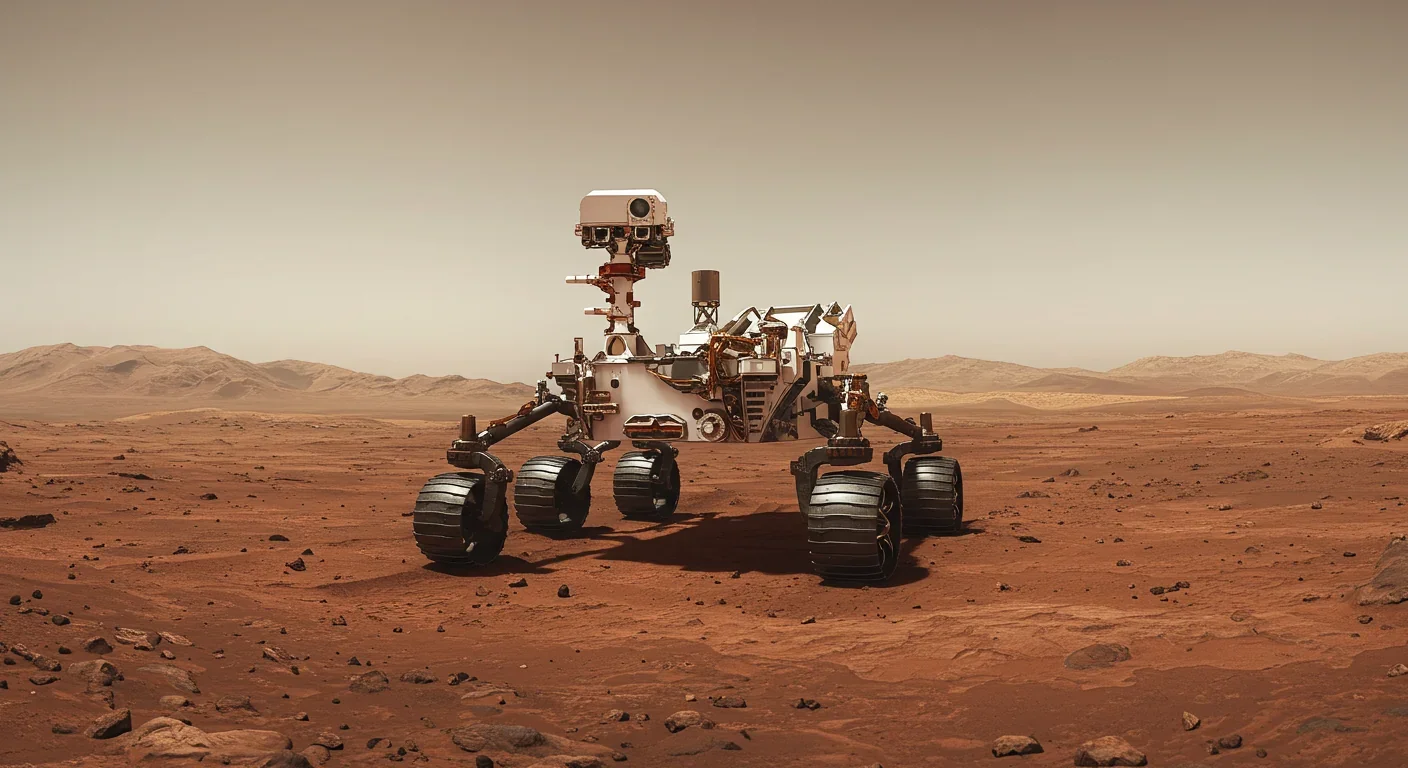
Curiosity rover detects mysterious methane spikes on Mars that vanish within hours, defying atmospheric models. Scientists debate whether the source is hidden microbial life or geological processes, while new research reveals UV-activated dust rapidly destroys the gas.

CMA is a selective cellular cleanup system that targets damaged proteins for degradation. As we age, CMA declines—leading to toxic protein accumulation and neurodegeneration. Scientists are developing therapies to restore CMA function and potentially prevent brain diseases.

Intercropping boosts farm yields by 20-50% by growing multiple crops together, using complementary resource use, nitrogen fixation, and pest suppression to build resilience against climate shocks while reducing costs.

The Baader-Meinhof phenomenon explains why newly learned information suddenly seems everywhere. This frequency illusion results from selective attention and confirmation bias—adaptive evolutionary mechanisms now amplified by social media algorithms.

Plants and soil microbes form powerful partnerships that can clean contaminated soil at a fraction of traditional costs. These phytoremediation networks use biological processes to extract, degrade, or stabilize toxic pollutants, offering a sustainable alternative to excavation for brownfields and agricultural land.

Renters pay mortgage-equivalent amounts but build zero wealth, creating a 40x wealth gap with homeowners. Institutional investors have transformed housing into a wealth extraction mechanism where working families transfer $720,000+ over 30 years while property owners accumulate equity and generational wealth.
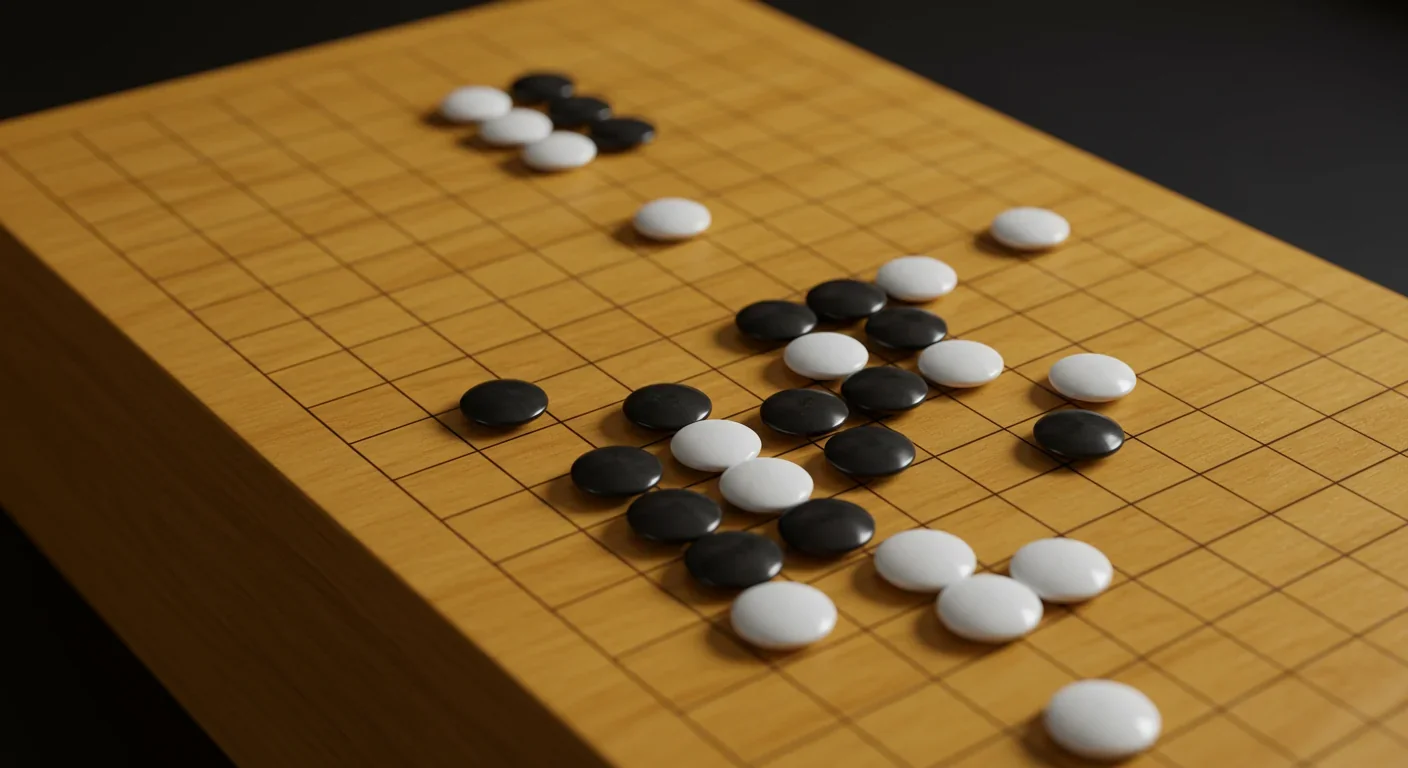
AlphaGo revolutionized AI by defeating world champion Lee Sedol through reinforcement learning and neural networks. Its successor, AlphaGo Zero, learned purely through self-play, discovering strategies superior to millennia of human knowledge—opening new frontiers in AI applications across healthcare, robotics, and optimization.