Your Cell's Protein Cleanup Fails With Age—Causing Brain Disease

TL;DR: Base editing, a molecular pencil that rewrites single DNA letters without cutting strands, has just saved its first patients and promises to cure thousands of genetic diseases—but society isn't ready for the ethical questions it raises.

By 2030, doctors predict thousands of genetic diseases once considered untreatable will be curable with a single therapy. The technology behind this transformation doesn't rely on cutting DNA like traditional gene editing. Instead, it works more like a molecular pencil, erasing single letters in our genetic code and replacing them with the correct ones. This breakthrough, called base editing, just saved its first patients—and it's about to change how we think about genetic disease forever.
A 21-year-old woman from Nigeria traveled to Shanghai in early 2025 with sickle cell disease so severe she suffered constant pain crises. Within 13 days of receiving a base editing therapy called CS-101, her bone marrow began producing healthy blood cells. By month three, her fetal hemoglobin levels soared above 60%—high enough to prevent the sickling that had tormented her for years. Six months later, she remained crisis-free with no adverse effects.
Around the same time, a five-month-old boy known as Baby KJ received a different kind of base editing treatment for a fatal liver disorder. His therapy was custom-designed and delivered in just seven months from diagnosis—a timeline once thought impossible for personalized gene therapy. KJ's success, along with an adult chronic granulomatous disease patient who received prime editing (an even more versatile form of base editing), marks what David Liu of Harvard calls "the Alyssa Tapley moment" for this technology. Just as Alyssa became the first person cured of leukemia with gene-edited immune cells, these patients represent the dawn of precision genetic medicine.
What makes these stories remarkable isn't just that the patients improved. It's how the editing happened—with surgical precision and none of the DNA damage that made earlier gene-editing approaches risky.
Your DNA is written in an alphabet of just four chemical letters: A, T, G, and C (adenine, thymine, guanine, and cytosine). These letters pair up in specific ways—A with T, G with C—to form the double helix. A single letter out of place in your three billion base pairs can cause catastrophic disease. Sickle cell disease stems from one A that should be a T. Many cases of cystic fibrosis trace to a three-letter deletion. Some cancers start when specific letters mutate in genes that control cell growth.
Traditional CRISPR-Cas9 gene editing works like molecular scissors. It cuts both strands of the DNA double helix at a target location, creating a break the cell must repair. Think of it as cutting a sentence out of a book with a razor blade, then hoping the printer's glue holds when you patch in the correction. The cell's repair machinery does fix the break, but the process is imperfect. Sometimes it deletes chunks of nearby DNA. Other times it inserts random fragments or rearranges chromosomes—like a photocopier that occasionally scrambles pages.
Base editors take a completely different approach. Instead of cutting DNA, they chemically convert one letter into another right where it sits in the genome. The editing machinery contains two key components: a modified Cas9 enzyme that binds to the target spot without cutting, and a deaminase enzyme that performs the actual chemical conversion. Cytidine base editors (CBEs) can change C to T (and therefore G to A on the opposite strand). Adenine base editors (ABEs) can switch A to G (and T to C). The system finds the exact genetic typo, transforms the incorrect letter into the correct one, and walks away—all without ever breaking the DNA strand.
It's the difference between erasing a pencil mark and rewriting it versus cutting a hole in the page.
When both strands of DNA break simultaneously, cells go into emergency mode. They deploy repair pathways designed for crisis management, not accuracy. One pathway, called non-homologous end joining (NHEJ), essentially glues the broken ends back together with little regard for what was there originally. Another, homology-directed repair (HDR), can incorporate a template you provide—but it only works in dividing cells and has low efficiency.
These repair processes create what scientists call "insertion-deletion mutations" (indels)—random additions or removals of genetic letters around the break site. In a coding region, indels often shift the reading frame of a gene, turning everything downstream into nonsense. Even when the desired edit succeeds, off-target cuts elsewhere in the genome can cause collateral damage. Large deletions spanning thousands of base pairs sometimes occur. Chromosomal rearrangements—where whole sections of DNA swap places—have been observed. While these events are rare, their potential to trigger cancer or disable essential genes makes regulators and clinicians understandably cautious.
Base editing sidesteps this entire problem. By making a chemical change to a single base without cleaving the DNA backbone, the technology avoids activating those error-prone repair pathways. The result, according to the team at CorrectSequence Therapeutics behind the CS-101 trial, is "efficient hematopoietic recovery and higher HbF-to-HbS ratio, without the risks of large DNA deletions, chromosomal rearrangements, or off-target mutations."
That safety profile matters enormously when you're editing cells destined to live in a patient's body for decades.
Sickle cell disease has become the proving ground for base editing. The CS-101 trial in China represents the world's first base editing therapy for beta-hemoglobinopathies. Instead of directly fixing the sickle cell mutation, CS-101 targets a regulatory element in the promoter of the gamma-globin genes. This reactivates fetal hemoglobin (HbF), which naturally doesn't sickle. By converting one base in this regulatory region, the therapy essentially flips a genetic switch that humans normally turn off in infancy. The patient's own bone marrow becomes a factory for protective hemoglobin without requiring wholesale replacement of the mutated adult hemoglobin gene.
Prime editing, developed in Liu's lab as an extension of base editing, goes further. In April 2023, Liu's team demonstrated that prime editing could restore the wild-type hemoglobin beta gene in cell models—something base editors alone couldn't accomplish. When these edited stem cells were transplanted into mice with sickle cell disease, long-term function returned with high clinical efficacy. By 2025, the first adult chronic granulomatous disease (CGD) patient received prime-edited bone marrow that restored enzyme activity with no serious adverse effects.
Progeria, a devastating accelerated-aging disorder caused by a single G-to-A mutation, offers perhaps the clearest proof that base editing works. In mouse models, base editing increased lifespan by a staggering 140%, according to research published in Nature. The mutation sits in a single letter of the LMNA gene. Because progeria is "caused by a change to a single letter in the DNA," the Progeria Research Foundation notes, "it is perfectly suited for this type of gene therapy."

Dravet syndrome, a severe form of epilepsy caused by mutations in the SCN1A gene, is also in base editing's crosshairs. Researchers are refining approaches to not only correct the genetic defect but also assess whether editing can reverse functional deficits in parvalbumin-expressing interneurons—the brain cells most critical to Dravet syndrome. If successful, this would demonstrate that base editing can do more than just fix DNA; it can restore lost neurological function.
Baby KJ's case showcases another dimension: speed. His custom base editing therapy moved from diagnosis to treatment in seven months. "The editing technology, the delivery technology, the manufacturing, the animal models, and the regulatory approval," David Liu explained, "are all robust enough to make this huge team effort happen fast enough to save Baby KJ."
The last technology that gave us this kind of power over human destiny was antibiotics. Before penicillin, a cut could kill you. Childbirth routinely ended in deadly infections. Tuberculosis hollowed out entire families. Then suddenly, in the span of a generation, bacterial infections became nuisances instead of death sentences. We went from helpless to nearly omnipotent over a category of disease.
Gene editing is poised to do the same for genetic disorders. Except this time, the transformation might happen faster. Antibiotics required decades of trial and error, mass production scale-up, and widespread clinical adoption. Base editing therapies are being designed on computers, tested in cell cultures, and validated in animals before ever reaching patients—compressing what used to take a career into a presidential term.
History also teaches caution. Antibiotics were initially hailed as miracle cures with no downsides. We deployed them so enthusiastically that we're now battling antibiotic-resistant superbugs. The lesson isn't that antibiotics were a mistake—they've saved hundreds of millions of lives. The lesson is that powerful tools need wise stewardship.
Base editing has been in development for less than a decade. David Liu's lab published the first base editor in Nature in 2016. We're already treating patients. That's faster than the jump from the Wright brothers' first flight to commercial aviation. It's faster than the leap from the first computer to the smartphone in your pocket. When a technology moves this quickly, society rarely has time to build the guardrails before the train is already moving.
Understanding base editing requires grasping three innovations that had to converge: CRISPR guidance, enzyme engineering, and delivery systems sophisticated enough to reach target cells.
CRISPR-Cas9 itself was revolutionary because it made gene editing programmable. Instead of engineering a new protein for every target gene, you simply design a short RNA guide that leads Cas9 to the right spot in the genome. Base editors inherit this programmability by using a modified Cas9 (either a nickase that cuts only one DNA strand, or a catalytically dead Cas9 that doesn't cut at all) fused to a deaminase enzyme.
The deaminase is where the magic happens. Cytidine deaminases convert cytosine to uracil, which cells then read as thymine during replication. Adenine deaminases (which took years longer to develop) convert adenine to inosine, read by cells as guanine. These are simple chemical transformations—removing an amino group here, adding a different one there—but they're irreversible without cellular intervention and highly specific when properly targeted.
Delivery remains the hardest problem. You can't just inject base editors into the bloodstream and hope they find their targets. For blood disorders like sickle cell, doctors extract a patient's stem cells, edit them in the lab, then reinfuse them after chemotherapy wipes out the original bone marrow—an arduous process requiring weeks of hospitalization. For brain disorders like Dravet syndrome, editors must cross the blood-brain barrier and reach neurons, which is far more challenging. Baby KJ received his therapy via direct injection into the liver during a surgical procedure.
Each delivery method has trade-offs. Ex vivo editing (outside the body) is safer because you can verify the edits before giving cells back to the patient. In vivo editing (inside the body) is more convenient but harder to control. Viral vectors can smuggle editors into cells efficiently but risk triggering immune responses. Lipid nanoparticles—the same technology behind COVID mRNA vaccines—offer a non-viral alternative that's showing promise.
Beam Therapeutics, a company co-founded by Liu, is tackling delivery challenges with engineered lipid nanoparticles designed to target specific organs. Verve Therapeutics is using base editing to lower cholesterol permanently by disabling the PCSK9 gene in the liver—a potential one-time treatment for heart disease that wouldn't require daily pills. These approaches hint at a future where gene editing could be administered as outpatient therapy, perhaps even as a simple injection.
Base editors excel at correcting point mutations—single-letter typos in the genetic code. Roughly 32,000 disease-causing mutations in the human genome are single-base changes that base editing could theoretically fix. This includes the mutations behind sickle cell disease, most cases of progeria, many instances of cystic fibrosis (though not all), hereditary deafness caused by GJB2 mutations, familial hypercholesterolemia, and some forms of muscular dystrophy.
But base editing has inherent limitations. Current base editors can only perform four types of conversions: C to T, T to C, A to G, and G to A. That covers transitions (changes within the same chemical family) but not transversions (changes between families, like C to G or A to C). Some disease mutations require transversions, putting them out of reach for base editing.
The technology also struggles with larger genetic problems. Deletions, duplications, and rearrangements that affect multiple bases or whole genes require different approaches. Duchenne muscular dystrophy, caused by large deletions in the dystrophin gene, is mostly beyond base editing's reach. Prime editing addresses some of these limitations by enabling insertions, deletions, and all 12 possible base-to-base changes, but it's less efficient than base editing and still being optimized.
Off-target effects remain a concern, though less severe than with CRISPR-Cas9. Base editors can occasionally modify unintended cytosines or adenines within the editing window (typically about 5 bases wide), leading to "bystander" edits. They can also cause off-target edits elsewhere in the genome if the guide RNA isn't perfectly specific. Researchers are improving targeting accuracy with high-fidelity base editors, better guide RNA design, and careful screening, but zero-risk editing doesn't exist yet.
RNA off-targets are another issue. Some base editors can modify RNA as well as DNA, potentially affecting gene expression in unpredictable ways. Newer base editor designs limit RNA editing, but it's still something researchers monitor carefully in preclinical testing.
Beyond sickle cell, progeria, and Dravet syndrome, base editing's potential stretches across medicine. Researchers are exploring treatments for:
Cardiovascular disease: Disabling PCSK9 or ANGPTL3 in the liver could permanently lower LDL cholesterol and triglycerides, preventing heart attacks and strokes without lifelong medication.
Cancer: Some cancers are driven by single-base mutations in oncogenes like KRAS or tumor suppressors like TP53. While editing cancer cells inside a tumor is challenging, base editing might prevent hereditary cancer syndromes by correcting mutations in healthy tissue.
Metabolic disorders: Phenylketonuria (PKU), caused by a mutation in the PAH gene, could be addressed by editing liver cells to restore enzyme function.
Hearing loss: The most common genetic cause of congenital deafness is a single mutation in GJB2. Base editing delivered to cochlear cells early in life might prevent hearing loss entirely.
Infectious disease: HIV-resistant cells could be created by editing CCR5 (the receptor HIV uses to infect cells) in a patient's immune cells. Chronic hepatitis B might be cured by inactivating viral DNA hiding in liver cells.
Neurological disorders: In addition to Dravet syndrome, conditions like Huntington's disease (caused by a CAG repeat expansion that base editing can't fix but prime editing might address) and some forms of Alzheimer's linked to APOE variants are under investigation.
The key constraint is delivery. Blood disorders are easiest because you can edit cells outside the body. Liver is accessible because it naturally takes up certain types of nanoparticles. Brain, muscle, and heart are far harder to reach. Unless delivery technology improves dramatically, some genetic diseases will remain out of base editing's reach for years or decades.
When thousands of genetic diseases become curable, society faces questions we've mostly postponed. If you can edit your future child's genome to remove a disease mutation, should you? What if you can also edit for height, intelligence, or athletic ability? Who decides which edits are medical necessities and which are enhancements?
The line isn't as clear as you'd think. Editing out the Huntington's disease mutation is obviously therapeutic. But what about editing APOE4 variants that increase Alzheimer's risk by two to three times? Is that treatment or prevention? What about PCSK9 editing to lower heart disease risk—is that medicine or enhancement if you don't currently have high cholesterol?
Some worry base editing will exacerbate inequality. These therapies are phenomenally expensive to develop and administer. CS-101 required extracting bone marrow, editing billions of cells, and transplanting them back after chemotherapy—a process that costs hundreds of thousands of dollars. Right now, only patients in clinical trials or those wealthy enough to pay out-of-pocket have access. If cures for genetic diseases remain exclusive to the rich, we'll create a biological class divide where some families can buy their way out of disease while others suffer preventable conditions.

Others counter that all medical technologies start expensive and niche before becoming widespread. The first antibiotics were scarce and costly. Now they're generic and ubiquitous. Insulin used to require grinding up pig pancreases; now it's manufactured in vats of engineered bacteria. If base editing follows that trajectory—and companies like Beam Therapeutics aim to make it so—today's $500,000 treatment could become a $5,000 outpatient procedure within a generation.
There's also the specter of unintended consequences. Our genome is staggeringly complex, with most genes affecting multiple traits and most traits influenced by many genes. Editing a base to fix one problem might create another down the line. The sickle cell mutation, for example, confers malaria resistance. Remove it from a population and you might inadvertently increase vulnerability to malaria in regions where the disease is endemic. Evolution doesn't create mutations out of malice. Sometimes what looks like a defect serves a hidden purpose.
Different cultures are approaching base editing with distinct philosophies that will shape how the technology unfolds globally.
China is moving aggressively. The CS-101 trial launched in Shanghai without the years of regulatory review typical in the US and Europe. China's 2019 law on human genetic resources explicitly promotes research on gene editing while banning heritable edits (changes that affect reproductive cells and could pass to future generations). The government sees gene editing as a strategic priority that could leapfrog Western dominance in biotech. It's investing billions in CRISPR research and has more gene-editing clinical trials underway than any other nation.
The United States takes a more cautious stance. The FDA requires extensive preclinical data before approving even early-phase trials. Heritable gene editing is effectively banned not by law but by the refusal of federal agencies to fund or review it. Yet the regulatory framework is comparatively flexible. When Baby KJ needed treatment, FDA approved his custom therapy under compassionate use provisions in record time—a pragmatism that balances safety with urgency.
Europe leans even more conservative. The European Medicines Agency (EMA) has rigorous standards for gene therapy approval. Some European nations view gene editing with deep suspicion rooted in memories of eugenics programs in the 20th century. Germline editing (editing embryos or reproductive cells) remains broadly forbidden. Somatic editing (editing non-reproductive cells) is allowed but tightly regulated.
In the Global South, perspectives vary wildly. Nigeria, home of the first CS-101 patient, sent her to China for treatment because base editing wasn't available domestically. Many developing nations lack the infrastructure for advanced gene therapies, creating a geographic lottery where your birthplace determines access to cures. Some see gene editing as a tool of neocolonialism, where wealthy nations test therapies on Global South populations before bringing them home. Others view it as a chance to leapfrog traditional healthcare limitations the same way mobile phones bypassed landline infrastructure.
Religious and philosophical traditions add another layer. Some branches of Christianity embrace gene therapy as a form of healing consistent with divine will. Others see editing human genomes as usurping God's role. Islamic scholars have debated whether gene editing constitutes permissible medical treatment or forbidden tampering with creation; many conclude it's acceptable for serious diseases but not for enhancement. Buddhist perspectives often emphasize the interconnectedness of life and caution against unintended harm to future generations.
Indigenous communities raise questions about collective genetic heritage. If a mutation prevalent in a specific population is edited out, does that erase part of their identity? Who consents to changes that could affect descendants?
Whether you're a patient, parent, or simply a human being with genes, base editing will affect your life. Here's how to prepare:
Stay informed but skeptical. Every new gene therapy will be hailed as a breakthrough. Some will deliver. Others will fail in late-stage trials or prove too expensive for widespread use. Learn enough molecular biology to distinguish hype from substance. Understand the difference between a mouse study, a Phase I safety trial, and an actual approved therapy.
Understand your genetic risks. As gene editing becomes viable, knowing which mutations you carry matters more. Direct-to-consumer genetic testing is imperfect, but it can flag whether you carry mutations for diseases like sickle cell, cystic fibrosis, or BRCA-related cancers. If you have a family history of genetic disease, genetic counseling can assess risk and options.
Engage in policy debates. Decisions about which gene edits should be allowed, who should pay for them, and whether we permit heritable editing will be made by legislatures and regulatory agencies over the next decade. If you don't participate, others will decide for you. That means voting for representatives who understand science, commenting on proposed regulations, and supporting organizations that advocate for equitable access.
Prepare for ethical gray zones. At some point you or someone you love will face a decision about gene editing. Maybe it's editing an embryo to remove Huntington's disease. Maybe it's editing an adult's liver to cure hepatitis B. These choices will be fraught. There won't be perfect answers. Cultivate the capacity to weigh trade-offs, tolerate uncertainty, and make decisions even when all options feel unsatisfying.
Support broad access. Technologies remain expensive when only a few people use them. If base editing is going to benefit humanity rather than just elites, we need public funding for research, price regulations to prevent profiteering, and global infrastructure to deliver therapies equitably. Advocate for policies that make cures accessible.
By 2035, doctors expect base editing to be routine for dozens of genetic diseases. By 2050, it could be as common as chemotherapy is today. That timeline means children being born now will grow up in a world where genetic diseases are increasingly optional.
We're not prepared for that world. Our legal systems still treat genes as immutable facts rather than editable code. Our insurance models assume disease is random rather than preventable through genetic intervention. Our ethical frameworks struggle to distinguish between fixing diseases and designing humans.
The first generation with access to widespread gene editing will have to invent the rules. They'll decide whether editing should stop at curing disease or extend to enhancement. They'll determine whether society funds gene therapies the way we fund vaccines or treats them as luxury medicine. They'll grapple with whether parents have the right to edit their children's genes—and if so, how far that right extends.
What we know for certain is that the molecular pencil is out of the drawer. We've started erasing genetic typos. Some of those edits will save lives. Others might create problems we haven't imagined yet. The technology isn't going back in the drawer. The question is how wisely we'll use it.
And whether we'll ensure everyone gets a pencil, or just those who can afford one.
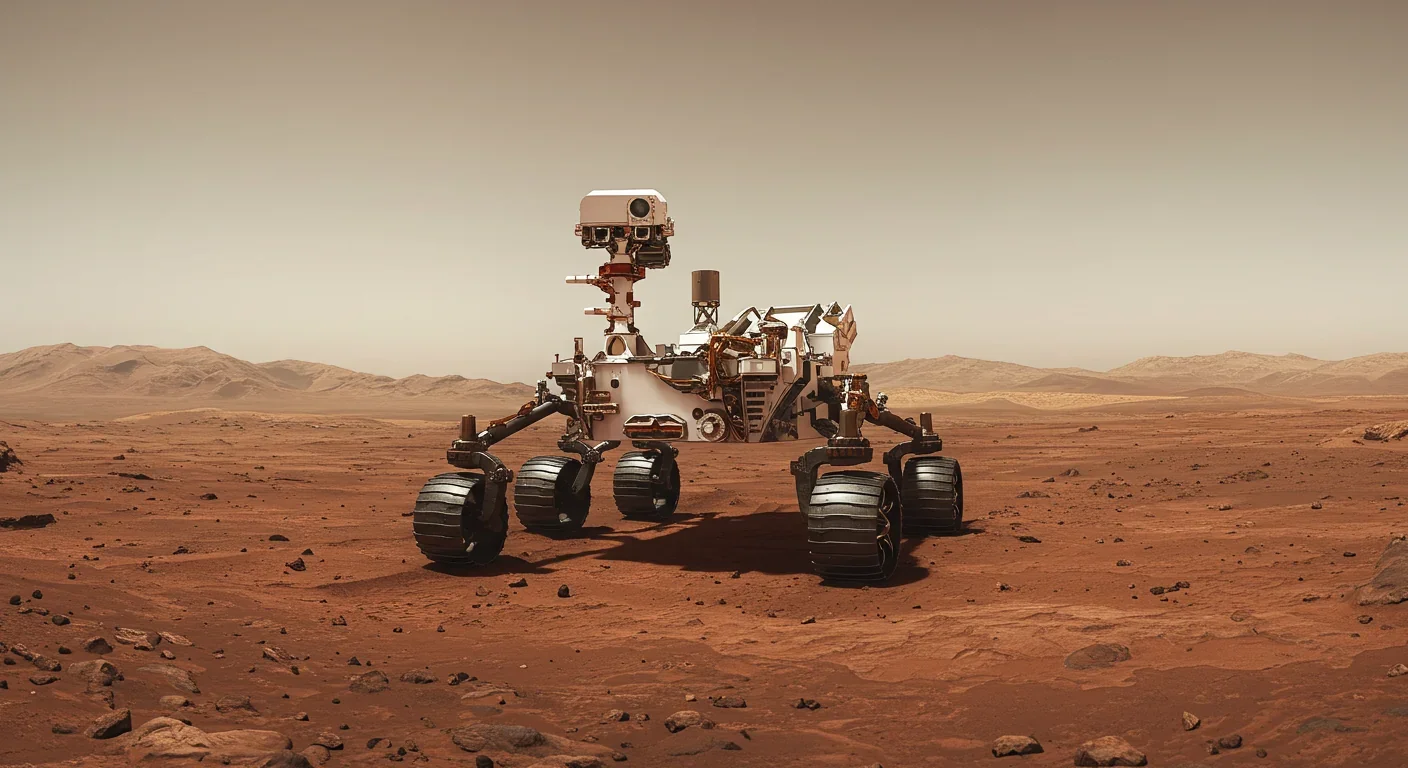
Curiosity rover detects mysterious methane spikes on Mars that vanish within hours, defying atmospheric models. Scientists debate whether the source is hidden microbial life or geological processes, while new research reveals UV-activated dust rapidly destroys the gas.

CMA is a selective cellular cleanup system that targets damaged proteins for degradation. As we age, CMA declines—leading to toxic protein accumulation and neurodegeneration. Scientists are developing therapies to restore CMA function and potentially prevent brain diseases.

Intercropping boosts farm yields by 20-50% by growing multiple crops together, using complementary resource use, nitrogen fixation, and pest suppression to build resilience against climate shocks while reducing costs.

The Baader-Meinhof phenomenon explains why newly learned information suddenly seems everywhere. This frequency illusion results from selective attention and confirmation bias—adaptive evolutionary mechanisms now amplified by social media algorithms.

Plants and soil microbes form powerful partnerships that can clean contaminated soil at a fraction of traditional costs. These phytoremediation networks use biological processes to extract, degrade, or stabilize toxic pollutants, offering a sustainable alternative to excavation for brownfields and agricultural land.

Renters pay mortgage-equivalent amounts but build zero wealth, creating a 40x wealth gap with homeowners. Institutional investors have transformed housing into a wealth extraction mechanism where working families transfer $720,000+ over 30 years while property owners accumulate equity and generational wealth.
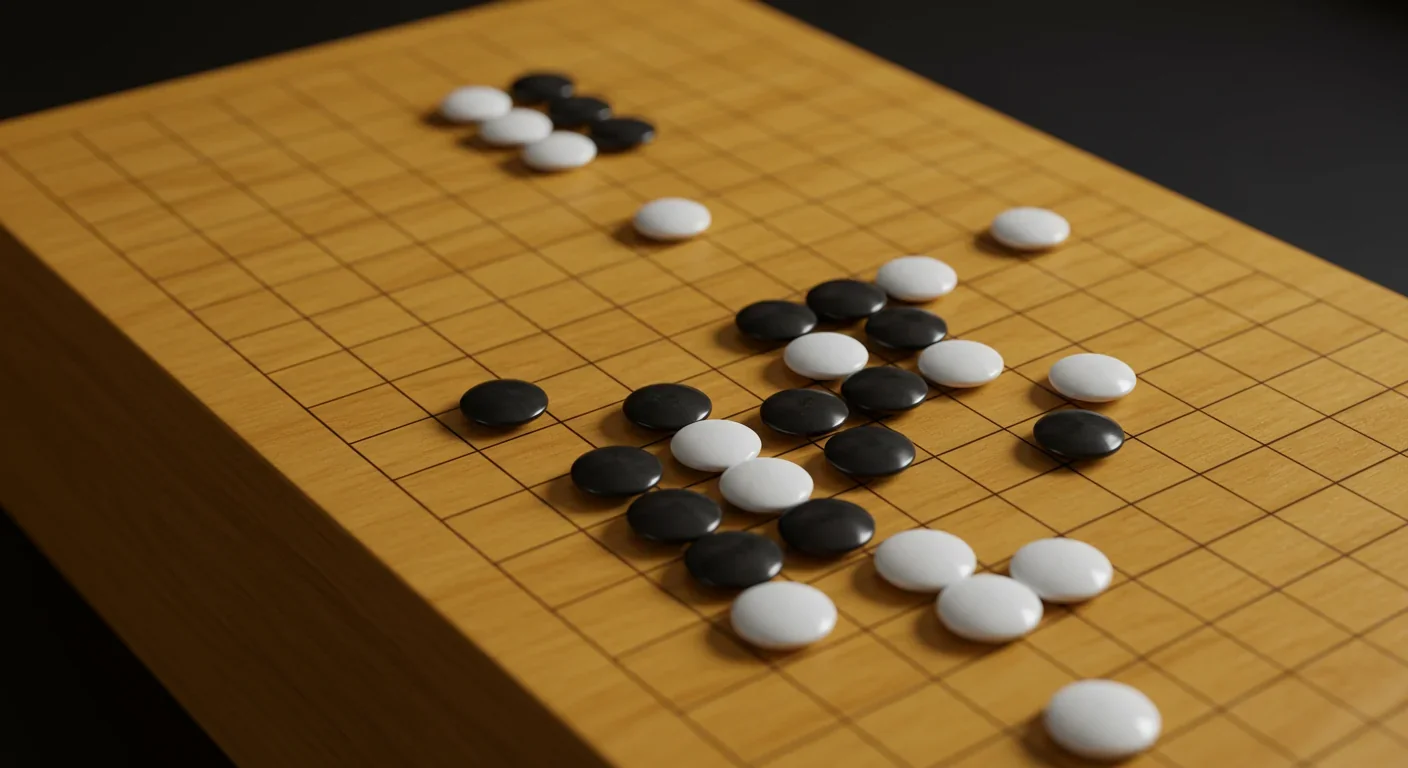
AlphaGo revolutionized AI by defeating world champion Lee Sedol through reinforcement learning and neural networks. Its successor, AlphaGo Zero, learned purely through self-play, discovering strategies superior to millennia of human knowledge—opening new frontiers in AI applications across healthcare, robotics, and optimization.