Your Cell's Protein Cleanup Fails With Age—Causing Brain Disease

TL;DR: Common gut bacterium Bacteroides fragilis produces a toxin (BFT) that damages intestinal barriers, triggers chronic inflammation, and promotes colorectal cancer in up to 88.5% of some patient populations. Scientists have identified a druggable target and potential prevention strategies.
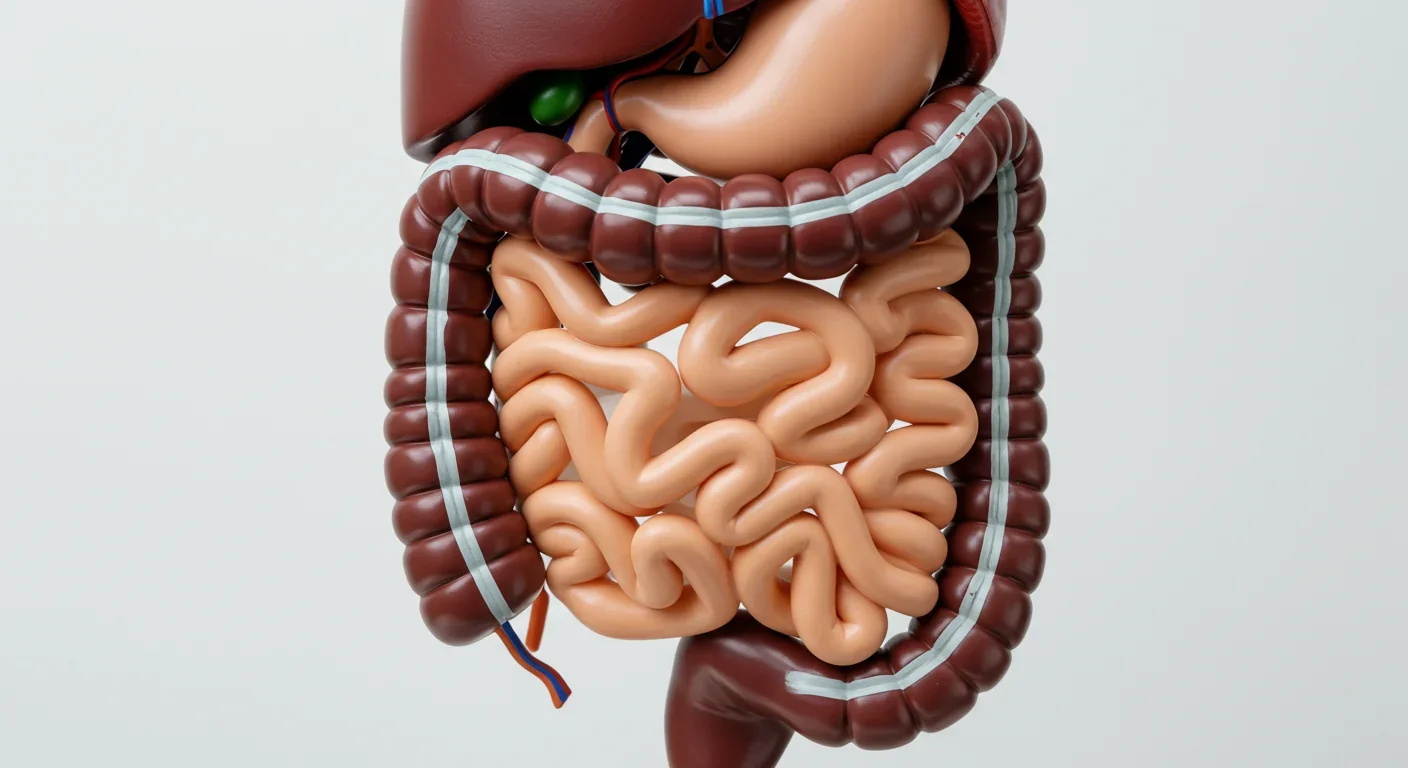
Within the next decade, your doctor might test your gut microbiome just as routinely as they check your cholesterol now. Recent research reveals that a common gut bacterium called Bacteroides fragilis, when it produces a specific toxin, could be secretly setting the stage for colorectal cancer in millions of people.
While most people think of bacteria as either good or bad, B. fragilis doesn't fit neatly into either category. This microbe lives in the guts of most healthy adults, quietly helping digest food and protect against pathogens. But a subset of these bacteria—called enterotoxigenic B. fragilis, or ETBF—produce a powerful protein called Bacteroides fragilis toxin (BFT) that can turn a helpful resident into a dangerous neighbor.
Scientists have found BFT in 41.6% of colorectal liver metastases and detected this toxin-producing strain in up to 88.5% of some colorectal cancer patient populations, compared with far lower rates in healthy controls. The numbers suggest we're looking at a major cancer trigger hiding in plain sight.
BFT is found in 41.6% of colorectal liver metastases, making it one of the most common bacterial factors in advanced cancer cases.
BFT operates like a molecular crowbar. This 21-kilodalton metalloprotease requires a zinc ion at its core to function, and when activated, it targets the adhesion proteins holding your intestinal cells together. The toxin specifically cleaves E-cadherin, the molecular glue that maintains the gut's protective barrier.
Think of your intestinal lining as a brick wall where each cell is a brick and E-cadherin is the mortar. BFT dissolves that mortar, causing cells to round up, swell, and separate. The result? Your gut barrier springs leaks, bacteria gain access to tissues they shouldn't touch, and chronic inflammation takes hold.
But the damage doesn't stop at barrier disruption. Once BFT breaches the epithelial wall, it kicks off a cascade of cellular changes that read like a cancer playbook. The toxin activates the Wnt/β-catenin pathway, a critical regulator of cell growth that, when dysregulated, drives uncontrolled proliferation. It also fires up NF-κB and STAT3 signaling, which crank out pro-inflammatory mediators like IL-17, IL-6, and TNF-α.
"BFT is a zinc-dependent metalloprotease toxin that disrupts cell junctions of E-cadherin and β-catenin, leading to increased intestinal permeability and inflammation."
— BMC Gastroenterology, Meta-Analysis
These aren't just abstract molecular pathways—they're the machinery that transforms normal cells into cancerous ones. BFT promotes DNA damage, ramps up the expression of oncogenes like c-Myc and cyclin D1, and recruits regulatory T cells and macrophages that suppress the immune response. In essence, the toxin creates an environment where tumor cells can thrive unchallenged.
Colorectal cancer doesn't appear overnight. It's the endpoint of years—sometimes decades—of cumulative damage. BFT-producing bacteria play the long game, establishing chronic inflammation that gradually erodes genetic stability.
Studies in mouse models show just how powerful this effect can be. When researchers colonize mice with ETBF and induce mild colitis, tumors form in as little as 12 weeks. Animals treated with non-toxigenic strains show a 70% reduction in polyp numbers, underscoring that it's the toxin—not just the bacterium—that matters.
In humans, the timeline is slower but the principle holds. High ETBF DNA levels in liver metastases correlate with increased densities of FOXP3+ regulatory T cells and CD68+ macrophages, both of which help tumors evade immune attack. ETBF doesn't just damage the original tumor site; it appears to shape the immune microenvironment of distant metastases, creating sanctuaries where cancer cells can flourish.

The toxin also induces spermine oxidase, an enzyme that generates reactive oxygen species (ROS). These ROS molecules inflict direct DNA damage, leading to mutations in critical tumor suppressor genes and oncogenes. Over time, this oxidative stress accelerates the transformation of healthy colon cells into malignant ones.
Not everyone harboring ETBF will develop colorectal cancer, but certain populations face higher odds. A recent meta-analysis found that colorectal cancer patients are 2.54 times more likely to carry ETBF than healthy controls. Prevalence varies significantly by region: West Asian populations show an odds ratio of 5.09, while European and American cohorts sit at 1.95, and East Asia registers a lower 1.10.
These geographic differences hint at the complex interplay of diet, genetics, and environmental factors. High-fat, low-fiber Western diets may favor ETBF colonization by altering gut pH and bile acid composition. Antibiotic use can disrupt the balance of commensal bacteria, allowing toxigenic strains to expand unchecked. And certain genetic variants may make some individuals' gut barriers more vulnerable to BFT's attacks.
Age is another factor. Colorectal cancer incidence rises sharply after 50, and so does the likelihood of ETBF colonization. Over decades, repeated exposure to BFT can accumulate mutations and epigenetic changes that eventually tip normal cells into malignancy.
Colorectal cancer patients are 2.54 times more likely to carry enterotoxigenic B. fragilis than healthy individuals, with regional variations reaching odds ratios as high as 5.09.
One of the frustrations in this field is the lack of standardized detection methods. Some studies use PCR to amplify the bft gene from stool samples, while others rely on tissue biopsies and immunohistochemistry. Detection rates vary wildly depending on the approach—tissue-based methods are generally more sensitive than stool tests, but they're also more invasive.
Emerging technologies promise to make detection easier. Droplet digital PCR can quantify ETBF DNA loads with high precision, even in archived formalin-fixed tissue. Next-generation sequencing allows researchers to map the entire gut microbiome, identifying not just ETBF but the broader microbial context that might promote or inhibit its growth.
Some scientists are developing microbial risk scores that integrate multiple bacterial species, including B. fragilis, into a single metric. One such score, based on α-diversity and the relative abundance of six core species, achieves AUCs (area under the curve) ranging from 0.619 to 0.824 across diverse patient cohorts. While not yet ready for clinical use, these tools could one day screen individuals at high risk long before symptoms appear.
Here's the surprising twist: nature may have already provided a countermeasure. Researchers discovered that chenodeoxycholic acid (CDCA), a bile acid currently used to treat gallstones and certain metabolic disorders, directly binds to BFT and blocks its catalytic site.
In lab tests, CDCA reduced BFT-induced morphological changes by 84% and slashed IL-8 secretion by 69%. The compound works by coordinating with the zinc ion at BFT's active site, essentially jamming the toxin's molecular machinery.
What makes this finding especially intriguing is that fecal CDCA concentrations vary naturally depending on gut transit time. People with faster colonic transit—such as those with diarrhea-predominant irritable bowel syndrome—have higher fecal CDCA levels. Could this explain why some individuals remain cancer-free despite carrying ETBF?
The therapeutic potential is real. CDCA is already approved for human use, shortening the path to clinical trials. And because it's a bile acid receptor agonist, it may offer dual benefits: inhibiting BFT while also dampening inflammation through FXR (farnesoid X receptor) signaling.
The BFT story challenges conventional approaches to cancer prevention. We've long focused on lifestyle factors like diet and exercise, and while those remain important, the microbiome adds a new dimension.
Imagine a future where routine colonoscopies include a stool sample analyzed for ETBF. High-risk individuals could receive targeted interventions—probiotics containing competitive, non-toxigenic B. fragilis strains, dietary modifications to lower gut pH, or even preemptive CDCA supplementation.
Probiotics are already being explored. Non-toxigenic B. fragilis strains can outcompete ETBF in the gut, reducing toxin production and inflammatory cytokine release. In animal models, these strains cut polyp formation by 70%, suggesting a promising avenue for human trials.

Dietary strategies matter too. Fiber-rich diets promote short-chain fatty acid production, which lowers colonic pH and inhibits pathogenic bacteria. Polyphenols from fruits and vegetables exhibit antimicrobial properties against ETBF. And fermented foods introduce beneficial microbes that can crowd out toxin-producers.
Antibiotic stewardship is critical. Broad-spectrum antibiotics wipe out commensal bacteria, creating ecological niches that ETBF can exploit. Clinicians should weigh the microbiome impact of antibiotic prescriptions, reserving them for situations where they're truly necessary.
BFT doesn't just damage cells—it manipulates the immune system. The toxin recruits regulatory T cells and tumor-associated macrophages, which suppress cytotoxic T cell activity and create an immunosuppressive microenvironment.
This immune modulation extends beyond the primary tumor. Studies show that liver metastases with high ETBF DNA loads have significantly more FOXP3+ regulatory T cells and CD68+ macrophages than metastases with low or no ETBF. The bacterium may actually help cancer cells establish distant outposts by preconditioning the metastatic niche.
Understanding this immune interplay could unlock new treatment strategies. Checkpoint inhibitors, which unleash the immune system against cancer, might work better in patients with high ETBF burdens if combined with BFT-targeted therapies. Reducing toxin levels could lift the immunosuppressive brake, allowing checkpoint inhibitors to do their job.
"ETBF colonization may contribute to an immune suppressive milieu in the metastatic tumor microenvironment."
— Saito et al. (2025), MDPI Cancers
Researchers are also exploring vaccines. If they can identify ETBF surface antigens that distinguish toxigenic from non-toxigenic strains, they might develop a vaccine that primes the immune system to eliminate ETBF before it causes harm.

The more scientists study ETBF, the more sophisticated it appears. Whole-genome sequencing of strains isolated from colorectal tumors reveals extensive horizontal gene transfer, genomic rearrangements, and virulence factors that help the bacterium thrive in hostile environments.
One key discovery: tumor-isolated ETBF strains carry type IV secretion system components, which facilitate toxin delivery into host cells. They also acquire capsule biosynthesis gene clusters that help evade immune detection and manage oxidative stress.
These genomic adaptations suggest that ETBF doesn't just passively colonize tumors—it actively evolves to exploit the tumor microenvironment. This arms race between host and microbe adds complexity but also opportunity. If we can disrupt the secretion systems or target the capsule biosynthesis pathways, we might render ETBF less virulent without killing off beneficial gut bacteria.
Translating these findings into clinical practice won't happen overnight. Clinical trials are needed to determine whether CDCA or other BFT inhibitors can reduce colorectal cancer incidence in high-risk populations. Longitudinal studies must establish whether ETBF colonization precedes tumor formation or simply accompanies it.
Standardized detection protocols are essential. Right now, researchers use different techniques, making it hard to compare results across studies. The field needs consensus on which genes to target, which sample types to use, and how to interpret positive results.
Regulatory hurdles also loom. Microbiome-based diagnostics and therapeutics exist in a gray zone between drugs and dietary supplements. Clear regulatory pathways will accelerate development and ensure that only effective interventions reach patients.
Still, progress is accelerating. Multiple biotech companies are developing microbiome-based cancer diagnostics. Academic groups are conducting pilot trials of probiotic interventions. And pharmaceutical firms are screening compound libraries for BFT inhibitors more potent than CDCA.
BFT isn't just a Western problem. While prevalence data remain patchy, studies from Greece, Denmark, China, Japan, and Iran all report substantial ETBF colonization in colorectal cancer patients. Yet no African studies appear in major meta-analyses, leaving a billion people largely unrepresented.
This data gap matters. Genetic diversity, dietary patterns, and endemic infections vary widely across populations, and these factors likely influence ETBF colonization and BFT-mediated carcinogenesis. Understanding regional differences could tailor prevention strategies and reveal protective factors unique to certain populations.
International collaboration is critical. Initiatives like the Human Microbiome Project and the International Cancer Microbiome Consortium are building global datasets that can identify universal versus population-specific risk factors. Such efforts will ensure that microbiome-based cancer prevention benefits everyone, not just those in high-income countries.

Major meta-analyses of BFT and colorectal cancer lack any data from Africa, leaving a billion people unrepresented in global prevalence estimates.
The discovery of BFT's role in colorectal cancer represents a paradigm shift. For decades, we've viewed cancer as a disease of our own cells gone rogue. Now we recognize that the trillions of microbes sharing our bodies can be co-conspirators.
This shift opens new avenues for prevention, early detection, and treatment. Imagine a world where a simple stool test identifies your cancer risk decades before symptoms appear. Where dietary tweaks or probiotics can neutralize that risk. Where drugs targeting bacterial toxins complement conventional chemotherapy and immunotherapy.
We're not there yet, but the pieces are falling into place. ETBF is detectable, BFT is druggable, and the biological mechanisms are increasingly clear. What's needed now is the will to translate these insights into practice—to fund large-scale trials, develop robust diagnostics, and educate clinicians and patients about the gut-cancer connection.
Colorectal cancer kills over 900,000 people worldwide each year. Many of those deaths are preventable if we catch the disease early or stop it before it starts. BFT research offers a tangible path forward, one that leverages our growing mastery of the microbiome to protect human health.
So the next time you think about cancer prevention, think beyond diet and exercise. Think about the invisible ecosystem inside you—and the bacterial toxins that might be plotting against your cells. Because understanding that hidden battleground could save your life.
Curiosity rover detects mysterious methane spikes on Mars that vanish within hours, defying atmospheric models. Scientists debate whether the source is hidden microbial life or geological processes, while new research reveals UV-activated dust rapidly destroys the gas.

CMA is a selective cellular cleanup system that targets damaged proteins for degradation. As we age, CMA declines—leading to toxic protein accumulation and neurodegeneration. Scientists are developing therapies to restore CMA function and potentially prevent brain diseases.

Intercropping boosts farm yields by 20-50% by growing multiple crops together, using complementary resource use, nitrogen fixation, and pest suppression to build resilience against climate shocks while reducing costs.

Cryptomnesia—unconsciously reproducing ideas you've encountered before while believing them to be original—affects everyone from songwriters to academics. This article explores the neuroscience behind why our brains fail to flag recycled ideas and provides evidence-based strategies to protect your creative integrity.

Cuttlefish pass the marshmallow test by waiting up to 130 seconds for preferred food, demonstrating time perception and self-control with a radically different brain structure. This challenges assumptions about intelligence requiring vertebrate-type brains and suggests consciousness may be more widespread than previously thought.

Epistemic closure has fractured shared reality: algorithmic echo chambers and motivated reasoning trap us in separate information ecosystems where we can't agree on basic facts. This threatens democracy, public health coordination, and collective action on civilizational challenges. Solutions require platform accountability, media literacy, identity-bridging interventions, and cultural commitment to truth over tribalism.

Transformer architectures with self-attention mechanisms have completely replaced static word vectors like Word2Vec in NLP by generating contextual embeddings that adapt to word meaning based on surrounding context, enabling dramatic performance improvements across all language understanding tasks.