Epigenetic Clocks Predict Disease 30 Years Early

TL;DR: Artificial organs grown from 3D-printed tissue and lab cultures are moving from science fiction to clinical reality, potentially eliminating transplant waiting lists within decades. But breakthroughs in vascularization and bioprinting bring profound challenges around access, ethics, and regulation.
By 2030, scientists predict that artificial organs could reduce transplant waiting lists by up to 40%, potentially saving hundreds of thousands of lives. Right now, someone dies every 10 minutes waiting for an organ donor. But in research labs across the globe, bioengineers are building replacement hearts, lungs, and kidneys from scratch—layer by microscopic layer, cell by living cell. What once belonged strictly to science fiction is becoming clinical reality, and the implications stretch far beyond medicine itself.
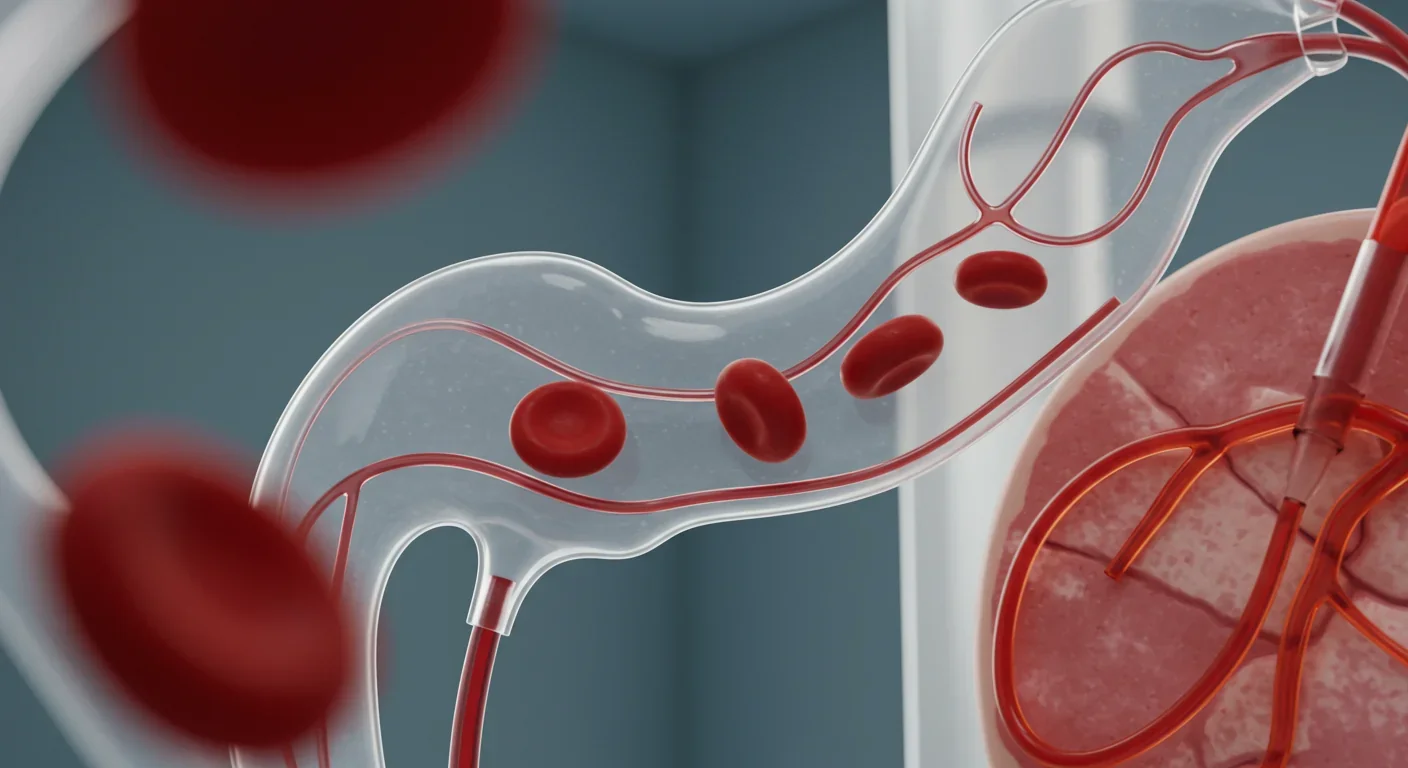
In 2023, U.S. surgeons performed 4,599 heart transplants—a record number, but still nowhere near enough. About 2,862 patients remained on the adult heart waiting list at year's end, with a mortality rate of 8.5 deaths per 100 patient-years. Meanwhile, researchers achieved something remarkable: they created artificial blood vessels using 3D bioprinting that could integrate with living tissue, solving one of the field's most stubborn challenges.
This wasn't just an incremental improvement. For decades, vascularization—the process of creating functional blood vessel networks—has been the major roadblock preventing lab-grown organs from working in real patients. Without blood flow, tissues die. The new 3D-printed artificial skin that allows blood circulation represents a fundamental shift in what's possible.
At the same time, xenotransplantation—using genetically modified pig organs in humans—crossed a crucial threshold. Surgeons completed the first pig-to-human lung transplant, demonstrating that organs from another species could function in a human body, at least temporarily. The technique is far from perfect, but it proved a concept that seemed impossible just a few years ago.
We've been trying to replace human body parts for centuries. Early attempts were crude: wooden legs, glass eyes, rudimentary prosthetics. In 1954, the first successful kidney transplant marked humanity's entry into the era of organ replacement using donor tissue. By the 1980s, cyclosporine and other immunosuppressants made transplants viable on a larger scale. But we hit a wall: demand always exceeded supply.
The idea of growing organs in labs emerged in the 1990s with tissue engineering efforts. Scientists cultured bladders, skin grafts, and cartilage, proving that human cells could be coaxed to form functional tissues outside the body. Yet complex organs—hearts, lungs, livers—remained out of reach because they require intricate internal structures, multiple cell types working in concert, and most crucially, blood vessels throughout.
3D printing technology, which became commercially available in the 2000s, offered a new approach. By the 2010s, researchers were bioprinting scaffolds that could guide cell growth into specific shapes. These weren't just molds; they were architectural frameworks that cells could colonize and transform into living tissue. The missing piece was always the same: vascularization.
Now, that piece is falling into place. Recent advances in bioprinting bone and cartilage organoids showed that researchers could create structures complex enough to support blood vessel formation. When combined with stem cell technology and genetic engineering, these developments are converging into a realistic pathway for creating fully functional artificial organs.
Creating a 3D-printed heart isn't like printing a plastic figurine. It's more like orchestrating a symphony where every instrument is a living cell. The process starts with imaging the patient's existing organ using CT or MRI scans to create a precise digital model. Bioengineers then use specialized printers that extrude "bio-inks"—mixtures of living cells, growth factors, and biocompatible materials—layer by layer.
The printer deposits these inks following the digital blueprint, building a three-dimensional scaffold that mimics the organ's structure. For a heart, this means creating chambers, valves, and crucially, a network of blood vessels ranging from large arteries down to tiny capillaries. The scaffold provides temporary support while the cells do their real work: multiplying, organizing, and gradually transforming into functional tissue.
Here's where it gets fascinating. Tiny 3D-printed devices can now deliver growth factors with unprecedented precision, essentially giving cells specific instructions about where to form blood vessels, when to differentiate into heart muscle, and how to connect with neighboring cells. Companies like Humacyte have developed engineered blood vessels that can be used in vascular surgery, demonstrating that the technology works for at least some tissue types.
Lab-grown lungs face even greater challenges because they require an elaborate branching structure—the bronchial tree—plus millions of microscopic air sacs called alveoli. But researchers have made progress using decellularization, where they strip cells from a donor lung (animal or cadaver), leaving just the structural framework. They then repopulate this scaffold with the patient's own cells, creating a lung that shouldn't trigger immune rejection. The first pig-to-human lung transplant used genetically modified pig organs to avoid hyperacute rejection, buying researchers time to study how the body responds.
If artificial organs become routine clinical practice, healthcare transforms entirely. The transplant waiting list—currently a death sentence for many—could disappear. No more rationing organs to the "most deserving" patients. No more debates about who gets bumped up the list. Instead, when your heart fails, you order a replacement grown from your own cells.
This scenario isn't purely hypothetical. The global tissue engineering market is projected to reach $170 billion by 2030, up from about $60 billion today. Investment is flooding into companies developing everything from bioprinted kidneys to engineered heart tissue for congenital defects.
Beyond transplants, artificial organs could revolutionize drug testing. Right now, pharmaceutical companies rely on animal testing and then clinical trials, a slow and expensive process where many promising drugs fail because human biology differs from mouse biology. Lab-grown human organs could serve as testing platforms, letting researchers see how drugs affect actual human tissue before ever entering clinical trials. This could accelerate drug development by years and make it far safer.
Surgical training would also transform. Instead of practicing on cadavers or learning on actual patients, surgeons could train on 3D-printed tissue that behaves like real organs, complete with realistic bleeding and responses to surgical tools. Medical schools could print organs on demand, customized to demonstrate rare conditions or anatomical variations.
Creating artificial organs is expensive now, but so are organ transplants. A heart transplant in the U.S. costs about $1.6 million, including pre-surgery evaluation, the operation itself, hospitalization, and a year of follow-up care. Patients then face lifetime expenses for immunosuppressant drugs, which can run $30,000 annually.
Artificial organs could eventually cost less because they eliminate many of these expenses. No need for immunosuppressants if the organ is grown from your own cells. No national organ procurement infrastructure. Reduced complications from rejection. The artificial organs market is expected to grow at 9.5% annually through 2032, suggesting investors believe the economics will work.
Manufacturing costs should fall dramatically with scale. Right now, bioprinting is artisanal—small batches in research labs. But companies are developing automated biofabrication systems that could mass-produce tissue constructs the way we manufacture electronics. When that happens, economies of scale kick in.
There's also massive potential for leapfrogging in developing countries. Nations without extensive organ donation infrastructure could skip straight to artificial organs, much as many African countries bypassed landline phones and went directly to mobile networks. The technology is modular—you need bioprinters, cell cultures, and trained technicians, but not the complex logistics of organ procurement and transport.
Here's the uncomfortable truth: every medical revolution begins as a luxury for the wealthy and slowly trickles down. In vitro fertilization, gene therapy, cancer immunotherapy—all started as treatments for the affluent. Artificial organs will probably follow the same trajectory.
Right now, only about 12% of U.S. heart transplant recipients have Medicare and 14.7% have Medicaid. The rest rely on private insurance or personal wealth. When artificial organs hit the market, they'll likely cost hundreds of thousands of dollars initially. Who gets access?
Globally, the disparities are even starker. Most organ transplants happen in wealthy countries with robust healthcare systems. Low-income nations perform few transplants not because their citizens don't need them, but because they lack infrastructure, resources, and often organ donation programs. Artificial organs won't automatically fix these inequities; they might deepen them initially.
There's another dimension to access: who owns the technology? If a handful of companies control the patents for bioprinting organs, they'll have immense pricing power. We've seen this play out with pharmaceuticals—lifesaving drugs priced beyond reach, creating massive ethical debates about profit versus human life. Intellectual property battles are already emerging as companies race to patent techniques, cell lines, and printing methods.
Some researchers advocate for open-source approaches where the technology remains freely available, allowing universities and hospitals worldwide to develop their own capabilities. Others argue that without patent protection, companies won't invest the billions needed for development. Finding the right balance will determine whether artificial organs become a tool for global health equity or another marker of inequality.
Optimism should be tempered with realism. Even if we solve the technical challenges, artificial organs introduce new risks and complications. Immunocompatibility remains imperfect. Using a patient's own cells reduces rejection risk but doesn't eliminate it entirely because the bioprinting process can alter cell behavior in unpredictable ways.
Cancers are another concern. Artificial organs require cells to multiply rapidly, and any time you accelerate cell division, you increase mutation risk. The scaffolding materials, growth factors, and culturing conditions could potentially create environments where cancerous cells emerge. Long-term studies will be essential.
Regulation presents its own challenges. The FDA's current framework for stem cell therapies and tissue engineering is evolving, but it wasn't designed for fully functional printed organs. How do you test a bioprinted heart before implanting it in a human? You can't exactly give it a test run. Phase I trials will be incredibly risky because there's no real animal model—pig hearts don't tell us enough about how a human heart will perform.
Xenotransplantation adds another layer of risk. Pigs carry viruses that don't affect them but might recombine with human viruses to create new pathogens. The pig-to-human lung transplant was groundbreaking but raises questions about disease transmission. We're potentially opening pathways for novel infections that could spread beyond the transplant recipient.
And then there's the ethics of enhancement. If we can print replacement organs, why not enhanced ones? A heart that never tires. Lungs with greater capacity. This isn't pure speculation—researchers in tissue engineering for congenital heart disease are already considering how to create improved versions of defective organs. The line between therapy and enhancement blurs quickly, raising profound questions about fairness, identity, and what it means to be human.
Different countries are taking remarkably different approaches to artificial organs, reflecting their values and healthcare systems. China has invested heavily in stem cell research and bioprinting, sometimes with less regulatory oversight than Western countries, allowing faster experimentation but also greater risk. Chinese researchers have made significant advances in 3D bioprinting bone and cartilage, often publishing results that seem ahead of Western equivalents.
Japan's approach emphasizes quality and safety, with stringent regulatory requirements but also government funding for regenerative medicine. The country faces an aging population and chronic organ shortages, creating urgency around finding alternatives to donor organs. Japanese regulators have shown willingness to approve regenerative therapies faster than the FDA, though still cautiously.
Europe splits the difference, with strong research programs balanced by ethical oversight. The European Union's regulatory framework requires extensive testing but also provides pathways for innovative therapies to reach patients. Countries like the Netherlands are using 3D printing in medical education, preparing the next generation of surgeons for a world where bioprinted organs are routine.
Religious and cultural perspectives also shape attitudes. Some religious traditions embrace artificial organs as extensions of healing, while others raise objections, particularly around xenotransplantation. Muslim scholars have debated whether pig-derived organs are permissible even if they save lives. Jewish bioethicists have generally endorsed the technology as falling under the principle of pikuach nefesh—preserving life overrides most other commandments. These aren't abstract debates; they determine whether billions of people will accept artificial organs as legitimate medical interventions.
This technology will arrive gradually, then suddenly. Within five years, expect to see limited clinical trials for bioprinted organs in desperate cases—patients who would otherwise die and have no other options. Within a decade, early commercial products will emerge for simpler organs: bladders, blood vessels, skin grafts. Within 15-20 years, hearts and lungs could become genuinely viable options.
What should you do with this knowledge? If you work in healthcare, start preparing now. Surgeons will need training in implanting artificial organs, which may behave differently than donor organs during surgery. Pathologists will need to interpret how bioprinted tissue responds to disease. Hospital administrators should consider infrastructure for storing and handling living tissue products.
If you're in policy or insurance, the questions multiply. Should artificial organs be covered the same way as donor organs? How do you price something that's part manufacturing and part medical procedure? What happens when wealthy patients can afford genetic enhancements in their printed organs while others can't?
For the rest of us, the implications are more personal. Think about advance directives and end-of-life planning. The equation changes when organ failure doesn't mean death. Consider whether you'd accept an artificial organ if needed, and whether you'd want it grown from your own cells or prefer a standardized version mass-produced for efficiency. These aren't hypothetical questions anymore.
The scientific challenges that remain are significant but not insurmountable. Researchers know what problems they need to solve: perfecting vascularization, eliminating rejection risks, ensuring long-term durability, streamlining production, reducing costs. Each year brings incremental progress. Sometimes, breakthroughs accelerate the timeline.
Artificial organs represent more than just medical advancement. They're a test of whether we can handle powerful technology responsibly, equitably, and ethically. We have a chance to avoid the mistakes of previous medical revolutions—the access inequities, the unintended consequences, the profit-over-patients dynamics.
The science is moving faster than our social and ethical frameworks. We need public discussions about who gets access, how we regulate safety without stifling innovation, and whether we want to draw lines between therapy and enhancement. These conversations should happen now, while the technology is still emerging, not after it's entrenched.
For patients on waiting lists, artificial organs offer hope after years of watching the clock tick down. For surgeons, they promise tools to save patients who currently die before a donor is found. For society, they raise fundamental questions about healthcare as a right versus a commodity, about enhancement versus treatment, about the price of progress.
The revolution in transplant medicine isn't coming. It's here, unfolding in research labs and early-stage trials. What remains to be seen is whether we'll build a future where these miracles of bioengineering serve everyone or just the fortunate few. That choice isn't up to scientists and engineers alone—it's up to all of us.

Recent breakthroughs in fusion technology—including 351,000-gauss magnetic fields, AI-driven plasma diagnostics, and net energy gain at the National Ignition Facility—are transforming fusion propulsion from science fiction to engineering frontier. Scientists now have a realistic pathway to accelerate spacecraft to 10% of light speed, enabling a 43-year journey to Alpha Centauri. While challenges remain in miniaturization, neutron management, and sustained operation, the physics barriers have ...

Epigenetic clocks measure DNA methylation patterns to calculate biological age, which predicts disease risk up to 30 years before symptoms appear. Landmark studies show that accelerated epigenetic aging forecasts cardiovascular disease, diabetes, and neurodegeneration with remarkable accuracy. Lifestyle interventions—Mediterranean diet, structured exercise, quality sleep, stress management—can measurably reverse biological aging, reducing epigenetic age by 1-2 years within months. Commercial ...

Data centers consumed 415 terawatt-hours of electricity in 2024 and will nearly double that by 2030, driven by AI's insatiable energy appetite. Despite tech giants' renewable pledges, actual emissions are up to 662% higher than reported due to accounting loopholes. A digital pollution tax—similar to Europe's carbon border tariff—could finally force the industry to invest in efficiency technologies like liquid cooling, waste heat recovery, and time-matched renewable power, transforming volunta...

Humans are hardwired to see invisible agents—gods, ghosts, conspiracies—thanks to the Hyperactive Agency Detection Device (HADD), an evolutionary survival mechanism that favored false alarms over fatal misses. This cognitive bias, rooted in brain regions like the temporoparietal junction and medial prefrontal cortex, generates religious beliefs, animistic worldviews, and conspiracy theories across all cultures. Understanding HADD doesn't eliminate belief, but it helps us recognize when our pa...

The bombardier beetle has perfected a chemical defense system that human engineers are still trying to replicate: a two-chamber micro-combustion engine that mixes hydroquinone and hydrogen peroxide to create explosive 100°C sprays at up to 500 pulses per second, aimed with 270-degree precision. This tiny insect's biochemical marvel is inspiring revolutionary technologies in aerospace propulsion, pharmaceutical delivery, and fire suppression. By 2030, beetle-inspired systems could position sat...

The U.S. faces a catastrophic care worker shortage driven by poverty-level wages, overwhelming burnout, and systemic undervaluation. With 99% of nursing homes hiring and 9.7 million openings projected by 2034, the crisis threatens patient safety, family stability, and economic productivity. Evidence-based solutions—wage reforms, streamlined training, technology integration, and policy enforcement—exist and work, but require sustained political will and cultural recognition that caregiving is ...

Every major AI model was trained on copyrighted text scraped without permission, triggering billion-dollar lawsuits and forcing a reckoning between innovation and creator rights. The future depends on finding balance between transformative AI development and fair compensation for the people whose work fuels it.