Epigenetic Clocks Predict Disease 30 Years Early

TL;DR: Nanorobots smaller than human cells are moving from labs to clinics, targeting diseases with microscopic precision. By 2033, this $12.44 billion market will transform how we fight cancer and infection, though manufacturing challenges and ethical questions remain.

By 2033, the global market for nanorobots in healthcare will reach $12.44 billion, a testament to one of medicine's quietest revolutions. Right now, inside research labs across North America, Europe, and Asia, scientists are perfecting microscopic machines smaller than a human cell that can navigate through your bloodstream, hunt down cancer cells, and deliver drugs with astonishing precision. These aren't science fiction fantasies, they're working prototypes that are already showing results in early trials.
At their core, nanorobots are submicroscopic devices typically measuring between 1 and 100 nanometers, about one-thousandth the width of a human hair. Most nanorobots currently in development rely on magnetic guidance systems that allow doctors to steer them through the body using external magnetic fields. Others use DNA origami, a technique where researchers fold DNA strands into precise three-dimensional shapes that can carry therapeutic payloads.
The technology works because these tiny machines can do what conventional drugs cannot: target specific cells while leaving healthy tissue untouched. When a cancer patient receives chemotherapy today, the drugs flood their entire system, killing both cancerous and healthy cells. DNA-based nanorobots from research teams at places like Karolinska Institutet can identify cancer cells by detecting specific proteins on their surfaces, then deliver cytotoxic agents only to those cells.
Björn Högberg, a leader in DNA nanotechnology, puts it bluntly: "DNA is not only a carrier of genetic information but also an excellent building material for nanoscale engineering." His team recently published research in Nature Nanotechnology demonstrating a DNA robotic switch that autonomously displays cytotoxic ligand nanopatterns, effectively creating a programmable assassin that only activates when it encounters its target.
The nanomedicine market reached $7.72 billion in 2025, driven primarily by targeted drug delivery applications. That dominance makes sense because gold nanoparticles have already demonstrated they can carry chemotherapy drugs like doxorubicin and paclitaxel directly to tumors in cervical and ovarian cancers. These particles, typically around 50 nanometers in diameter, can be synthesized using established methods that give researchers precise control over size, shape, and surface chemistry.
What makes gold nanoparticles particularly useful is their versatility. They function as both delivery vehicles and imaging agents. Radioiodinated gold nanoparticles serve as contrast agents for MRI, ultrasound, CT, and PET scans, allowing doctors to track exactly where the treatment is going in real time. Some formulations also enable photothermal therapy, where doctors shine near-infrared light on the tumor site, causing the nanoparticles to heat up and cook cancer cells from within.
Real-world applications extend beyond cancer. Researchers recently developed a nanomaterial-mediated antibiotic delivery system specifically for osteomyelitis, a bone infection that's notoriously difficult to treat because antibiotics struggle to penetrate bone tissue. The nanocarriers achieve site-specific accumulation and controlled release, concentrating the antibiotic exactly where it's needed while reducing systemic exposure.
The numbers tell the story of accelerating progress. Duke University's TuNa-AI platform recently generated a dataset of 1,275 distinct nanoparticle formulations, testing different therapeutic molecules, excipients, and ratios. AI-guided design achieved a 42.9% higher success rate in forming stable nanoparticles compared to conventional methods, and AI-optimized nanobots deliver drugs at tissue concentrations three to five times higher than traditional formulations.
Scaling nanorobot production from laboratory batches to millions of doses presents substantial hurdles. DNA nanorobots require positioning molecules with nanometer precision, a feat that's straightforward in controlled lab conditions but difficult to reproduce at commercial scale. The synthesis methods vary widely: some teams use the Turkevich citrate reduction for gold nanoparticles, others employ biological synthesis using plant or microbial extracts, and still others turn to physical approaches like laser ablation.
Each method produces particles with different characteristics. Laser-ablated gold quantum dots, for instance, generate 1-5 nanometer particles with minimal aggregation and higher photothermal efficiency than chemically synthesized versions. But laser ablation is expensive and challenging to scale. Chemical methods are cheaper but can introduce contaminants that trigger immune responses.
Quality control becomes exponentially more complex at the nanoscale. A batch of nanoparticles needs consistent size distribution, uniform surface coating, and reliable drug-loading efficiency. Even small variations can dramatically affect how the particles behave in the body. PEGylation, the process of coating nanoparticles with polyethylene glycol to shield them from immune detection, must be applied uniformly or some particles will be cleared from the bloodstream before reaching their target.
Storage and stability present additional problems. Many nanoparticle formulations are sensitive to temperature, light, and pH changes. Silver nanoparticles, for example, release silver ions continuously, with one formulation releasing 87 micrograms per milliliter after one day and 371 micrograms per milliliter after one week. That variability makes dosing unpredictable unless storage conditions are meticulously controlled.
The immune system treats nanoparticles like invading pathogens, which creates both problems and opportunities. When nanoparticles enter the bloodstream, the body's reticuloendothelial system, a network of immune cells in the liver and spleen, immediately begins clearing them. Within minutes, many nanoparticles are captured and destroyed before they reach their intended target.

Recent research suggests this immune response might be useful. Scientists at the University of Pennsylvania discovered that interferon-lambda, a protein induced by nanoparticle administration, reduces systemic clearance of subsequent nanoparticle doses without affecting tumor uptake. When they co-administered interferon lambda with nanoparticle-encapsulated chemotherapy in mice with colon cancer, the animals lived longer and lost less weight than those receiving chemotherapy alone.
This finding flips conventional wisdom. Instead of trying to hide nanoparticles from the immune system, researchers might be able to prime the immune system to tolerate them. The challenge lies in predicting which patients will develop strong immune responses and adjusting treatments accordingly.
Targeting accuracy remains imperfect. Even the most sophisticated nanorobots occasionally miss their mark or accumulate in unintended tissues. Hepatotoxicity from nanoparticle-based cancer drugs remains a concern because the liver naturally filters particles from the blood. Researchers have found that PEGylation reduces liver uptake by shielding nanoparticles from immune recognition, but it's not a perfect solution.
Some of the most promising developments involve hijacking the body's natural delivery systems. Exosomes, tiny vesicles that cells naturally release to communicate with each other, can be genetically engineered to display tumor-targeting peptides. When researchers fuse these peptides with Lamp2b, a protein found on exosome surfaces, the resulting biohybrid nanorobots home in on specific cancer cells with remarkable accuracy.
The FDA regulates nanomaterials in medical products but doesn't provide detailed reproductive safety protocols, leaving a regulatory gray zone that complicates clinical trials. Standard drug safety testing wasn't designed for particles that can cross biological barriers conventional drugs cannot. Nanoparticles can potentially cross the placental barrier, accumulate in fetal tissue, and cause developmental effects that won't appear for years.
Beyond biological safety, ethical questions abound. Who gets access to these treatments first? The concentration of nanorobotics research in North America, driven by advanced research infrastructure and stable R&D funding, risks creating a healthcare divide where cutting-edge treatments remain available only to wealthy patients in developed nations. Asia Pacific is catching up fast, with countries investing heavily in manufacturing capacity and clinical trials, but the gap persists.
Biocompatibility testing requirements for medical devices don't fully address nanoparticle-specific risks. Standard tests might miss toxic effects that only appear when particles accumulate in certain organs over months or years. Some researchers advocate for long-term monitoring programs that track patients for decades after treatment, but that approach would dramatically slow the path to market.
Informed consent becomes complicated when scientists themselves don't fully understand long-term risks. How do you explain to a cancer patient that a treatment might save their life today but could potentially cause unforeseen problems in twenty years? The urgency of terminal illness often pushes both doctors and patients to accept risks they might otherwise reject.
North America dominates the nanorobots healthcare market today, but that leadership is contested. Japan's nanorobotics sector includes major players like Hitachi, Sony, and Toshiba, companies with deep expertise in precision manufacturing and miniaturization. Europe contributes fundamental research through institutions like Karolinska Institutet, while China invests billions in nanotechnology research as part of its strategic plan to lead advanced manufacturing.
This geographic competition drives innovation but also creates coordination problems. International standards for nanorobot safety and efficacy remain underdeveloped. A nanoparticle formulation approved in one country might face different requirements elsewhere, slowing global adoption and fragmenting research efforts.
Different cultures bring different perspectives to the ethical questions. Some societies prioritize collective health benefits over individual autonomy, which could lead to faster adoption of promising technologies with uncertain long-term risks. Others emphasize precautionary principles, demanding extensive safety data before approving new treatments. Neither approach is obviously superior, but the tension between them shapes how quickly nanomedicine moves from laboratory to clinic.
Intellectual property battles are already heating up. Companies and universities are filing thousands of patents covering everything from basic nanoparticle synthesis methods to specific targeting ligands and drug combinations. This patent thicket might eventually stifle innovation if licensing becomes too complex or expensive, but for now it reflects the enormous commercial potential researchers see in the field.
Within the next decade, nanomedicine will likely shift from experimental therapy to standard treatment for certain cancers and chronic diseases. That transition will require changes throughout the healthcare system. Doctors will need training to understand which patients are good candidates for nanorobot treatments and how to monitor for complications. Pharmacists will need new protocols for handling and dispensing nanoparticle formulations. Hospitals will need imaging equipment capable of tracking nanorobots in real time.

Patients should start asking questions now. When diagnosed with cancer or another serious illness, it's worth investigating whether clinical trials involving nanomedicine are available. ClinicalTrials.gov lists ongoing studies, though navigating the database requires patience. Your doctor might not be familiar with the latest nanorobot research, so bringing published studies to appointments can help start informed conversations.
The cost trajectory remains uncertain. Manufacturing complexity suggests nanorobot treatments will initially be expensive, potentially limiting access to patients with comprehensive insurance or substantial personal wealth. But economies of scale could eventually drive prices down, especially if multiple companies compete to produce similar formulations. Government negotiation over pricing will shape whether these treatments become widely accessible or remain boutique options for the privileged.
Skills worth developing include basic understanding of nanotechnology principles, the ability to evaluate scientific claims critically, and comfort with statistical concepts like confidence intervals and p-values. As nanomedicine marketing inevitably ramps up, distinguishing genuine breakthroughs from incremental improvements will require some scientific literacy.
The nanorobots healthcare market is projected to grow at 6.15% annually through 2033, suggesting steady but not explosive expansion. That measured pace reflects the genuine challenges remaining: manufacturing scale-up, regulatory approval processes, long-term safety monitoring, and cost management all take time to resolve.
Magnetically controlled nanorobots currently dominate because external magnetic fields provide reliable, real-time steering without requiring complex onboard power sources. But next-generation designs might incorporate chemical propulsion systems or harness biological motors, potentially enabling more autonomous operation and better tissue penetration.
Combination approaches look particularly promising. Imagine nanorobots that simultaneously deliver chemotherapy, release immune-stimulating molecules to help the body's own defenses recognize cancer, and report back via imaging agents on treatment effectiveness. These multifunctional platforms are already being tested in animal models, and human trials aren't far behind.
The convergence of artificial intelligence and nanomedicine could accelerate progress dramatically. Machine learning algorithms are already designing better nanoparticle formulations faster than human researchers could. As AI systems gain access to more clinical data, they might identify patient characteristics that predict who will respond best to specific nanorobot treatments, enabling truly personalized nanomedicine.
Synthetic biology is opening new frontiers. Researchers are creating DNA nanorobots that can modify synthetic cells, potentially enabling treatments that reprogram diseased tissue at the cellular level. These approaches blur the line between therapy and enhancement, raising questions about how far we should go in reengineering human biology.
The most profound impact might be psychological. Growing up in a world where microscopic robots patrol your bloodstream, repairing damage and fighting disease before symptoms appear, fundamentally changes how we think about health and mortality. Today's children might never experience cancer as a death sentence, instead viewing it as a manageable chronic condition controlled by their personal fleet of nanorobots.
That future isn't guaranteed. Technical obstacles could prove insurmountable, unexpected toxicities might emerge, or public backlash against "unnatural" treatments could slow adoption. But the research momentum is undeniable. Thousands of scientists worldwide are betting their careers on making nanomedicine work, backed by billions in funding from governments, universities, and private companies.
We stand at the threshold of a transformation in how humans combat disease. The tiny warriors are coming, and they're bringing a revolution with them.
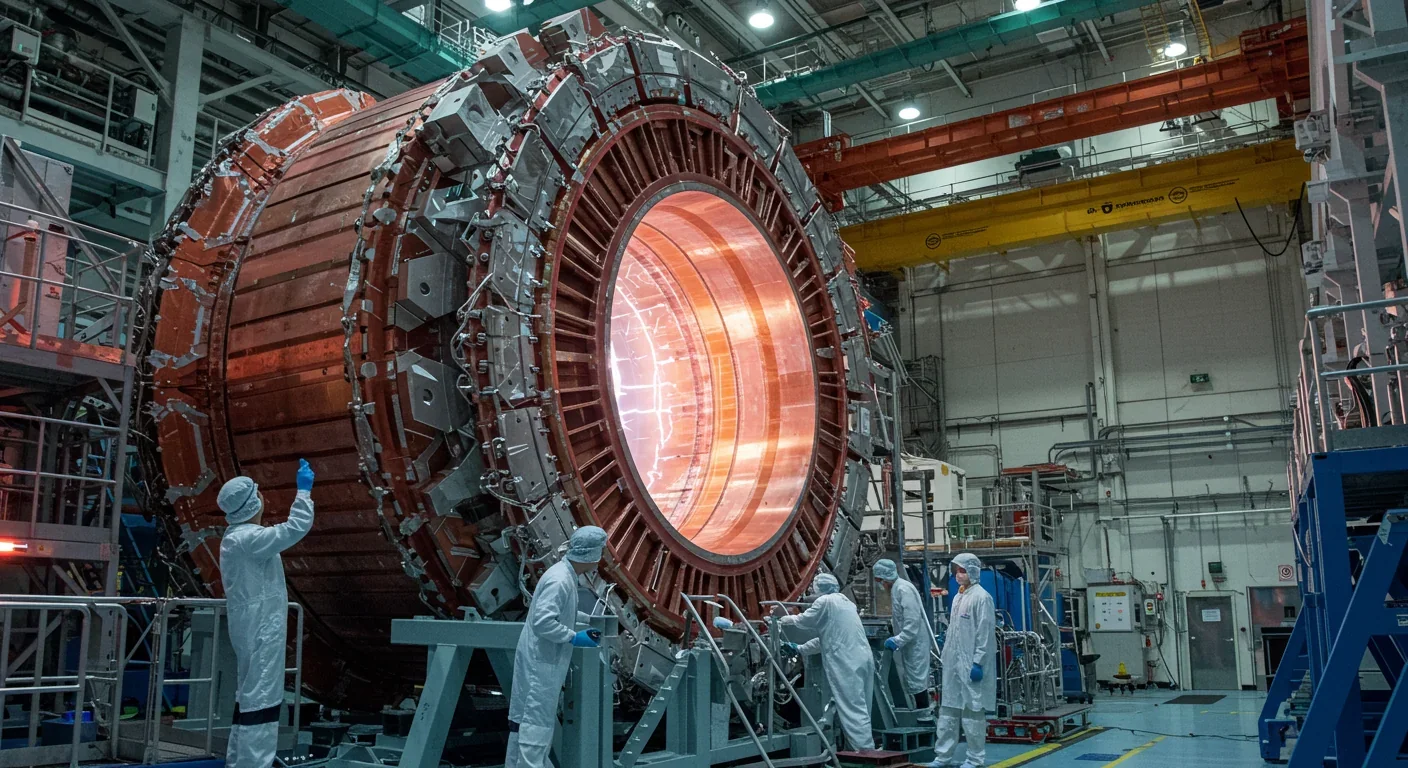
Recent breakthroughs in fusion technology—including 351,000-gauss magnetic fields, AI-driven plasma diagnostics, and net energy gain at the National Ignition Facility—are transforming fusion propulsion from science fiction to engineering frontier. Scientists now have a realistic pathway to accelerate spacecraft to 10% of light speed, enabling a 43-year journey to Alpha Centauri. While challenges remain in miniaturization, neutron management, and sustained operation, the physics barriers have ...

Epigenetic clocks measure DNA methylation patterns to calculate biological age, which predicts disease risk up to 30 years before symptoms appear. Landmark studies show that accelerated epigenetic aging forecasts cardiovascular disease, diabetes, and neurodegeneration with remarkable accuracy. Lifestyle interventions—Mediterranean diet, structured exercise, quality sleep, stress management—can measurably reverse biological aging, reducing epigenetic age by 1-2 years within months. Commercial ...

Data centers consumed 415 terawatt-hours of electricity in 2024 and will nearly double that by 2030, driven by AI's insatiable energy appetite. Despite tech giants' renewable pledges, actual emissions are up to 662% higher than reported due to accounting loopholes. A digital pollution tax—similar to Europe's carbon border tariff—could finally force the industry to invest in efficiency technologies like liquid cooling, waste heat recovery, and time-matched renewable power, transforming volunta...

Humans are hardwired to see invisible agents—gods, ghosts, conspiracies—thanks to the Hyperactive Agency Detection Device (HADD), an evolutionary survival mechanism that favored false alarms over fatal misses. This cognitive bias, rooted in brain regions like the temporoparietal junction and medial prefrontal cortex, generates religious beliefs, animistic worldviews, and conspiracy theories across all cultures. Understanding HADD doesn't eliminate belief, but it helps us recognize when our pa...

The bombardier beetle has perfected a chemical defense system that human engineers are still trying to replicate: a two-chamber micro-combustion engine that mixes hydroquinone and hydrogen peroxide to create explosive 100°C sprays at up to 500 pulses per second, aimed with 270-degree precision. This tiny insect's biochemical marvel is inspiring revolutionary technologies in aerospace propulsion, pharmaceutical delivery, and fire suppression. By 2030, beetle-inspired systems could position sat...

The U.S. faces a catastrophic care worker shortage driven by poverty-level wages, overwhelming burnout, and systemic undervaluation. With 99% of nursing homes hiring and 9.7 million openings projected by 2034, the crisis threatens patient safety, family stability, and economic productivity. Evidence-based solutions—wage reforms, streamlined training, technology integration, and policy enforcement—exist and work, but require sustained political will and cultural recognition that caregiving is ...

Every major AI model was trained on copyrighted text scraped without permission, triggering billion-dollar lawsuits and forcing a reckoning between innovation and creator rights. The future depends on finding balance between transformative AI development and fair compensation for the people whose work fuels it.