Epigenetic Clocks Predict Disease 30 Years Early

TL;DR: Synthetic blood substitutes are engineered oxygen carriers that could solve global blood shortages by providing universal, shelf-stable alternatives to donated blood. While regulatory and safety challenges remain, market projections show the field will grow from $9.73 billion to $46.37 billion by 2034.
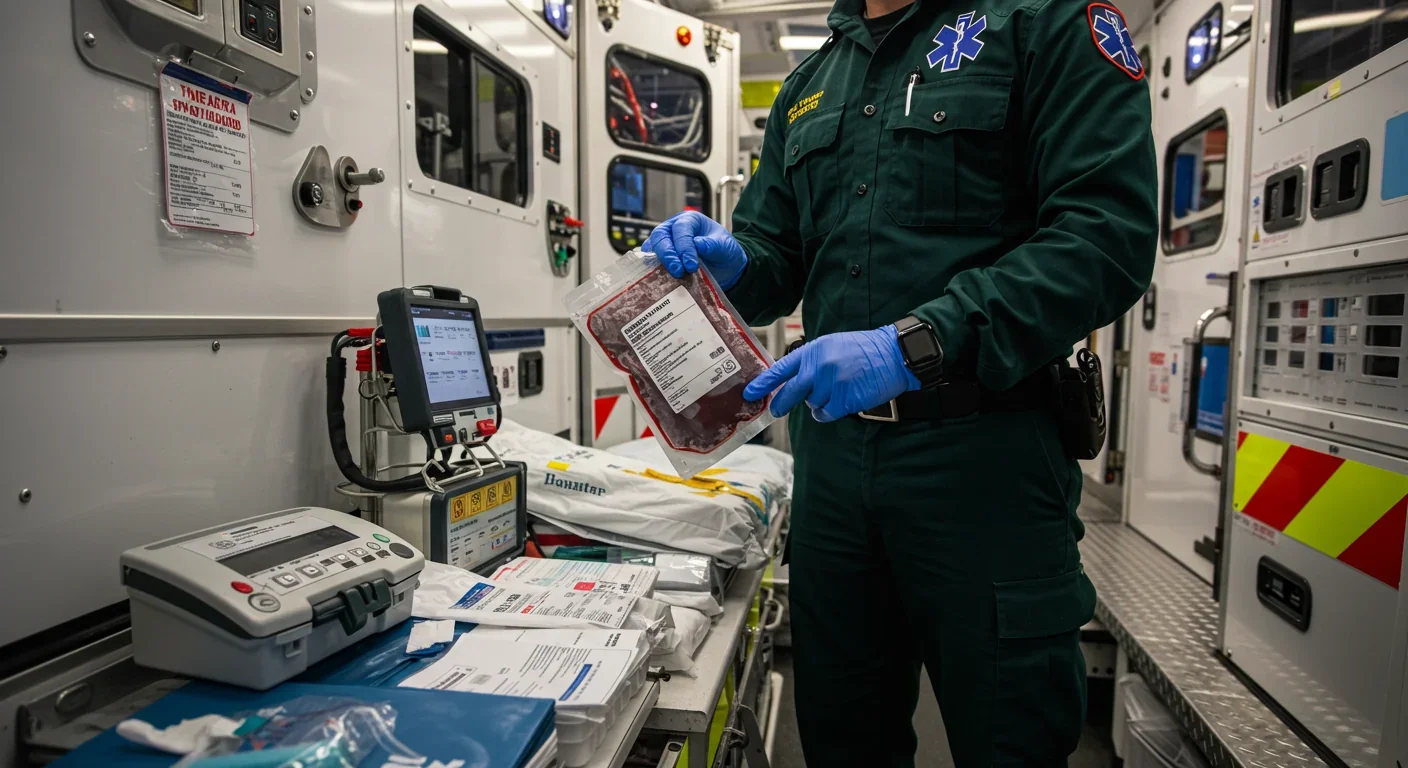
Every two seconds, someone in the United States needs blood. Yet across the globe, blood banks are running dry at an alarming rate. Traditional blood supplies depend on a shrinking pool of donors, logistical nightmares around storage and transport, and the perpetual race against expiration dates. But what if we could manufacture blood in a lab—free from disease, available on demand, and compatible with any patient? That future is closer than you think, and it's about to reshape emergency medicine forever.
Synthetic blood substitutes, technically called artificial oxygen carriers, don't replicate every function of human blood. They can't clot wounds, fight infections, or regulate body temperature. What they can do—brilliantly—is carry oxygen to your tissues when you're bleeding out on an operating table or trapped in a war zone thousands of miles from the nearest blood bank.
Scientists have developed two main types of these oxygen carriers. Hemoglobin-based oxygen carriers, or HBOCs, use modified hemoglobin molecules extracted from expired human blood or animal sources (usually cows). These molecules get chemically altered through processes like cross-linking and PEGylation to prevent them from breaking down too quickly in your bloodstream or stealing nitric oxide from your blood vessels—a dangerous side effect that plagued early versions.
The second type, perfluorocarbon-based oxygen carriers (PFCs), takes a completely different approach. These synthetic compounds, built from carbon and fluorine atoms, can dissolve up to 100 times more oxygen than your blood plasma. They're inert, colorless liquids that essentially act as microscopic scuba tanks floating through your veins, picking up oxygen in your lungs and releasing it wherever your body needs it most.
The numbers tell a sobering story. Demand for blood transfusions has reached unprecedented levels, driven by aging populations in developed countries, complex surgical procedures, and chronic diseases requiring regular transfusions. Meanwhile, the donor pool keeps shrinking. Younger generations donate at lower rates than their parents, and strict eligibility requirements disqualify millions of potential donors.
The problem gets worse when you look beyond wealthy nations. In conflict zones, remote areas, and developing countries, refrigerated blood storage is often impossible. Natural disasters and mass casualty events can exhaust local supplies within hours. Even in well-equipped hospitals, blood typing and cross-matching take precious time that trauma patients don't have.
Recent scandals have exposed another vulnerability. An outbreak in Iraq saw dozens of children contract HIV from contaminated blood transfusions, a nightmare scenario that synthetic substitutes could help prevent. Because lab-grown oxygen carriers can be manufactured under sterile conditions and don't carry human pathogens, they offer an extra layer of safety that donated blood simply can't match.
Understanding how synthetic blood functions requires looking at what makes natural blood so effective. Red blood cells contain roughly 270 million hemoglobin molecules each. Every hemoglobin molecule can grab four oxygen atoms in your lungs and ferry them to oxygen-starved tissues throughout your body. It's an elegant system refined over hundreds of millions of years of evolution.
But when you extract hemoglobin from red blood cells and inject it directly into someone's bloodstream, problems emerge fast. Free-floating hemoglobin molecules are tiny—so small that your kidneys filter them out within hours, potentially causing kidney damage. They also bind to nitric oxide, a molecule your blood vessels need to stay relaxed and open. Without enough nitric oxide, your blood pressure spikes dangerously.
Early researchers tried cross-linking hemoglobin molecules together to make them bigger and coating them with polyethylene glycol (PEG) to shield them from the immune system and slow their breakdown. These modifications worked to some extent, but they introduced new complications. Cross-linked hemoglobin tends to have such a tight grip on oxygen that it won't release the goods when tissues need it. Engineers had to tinker with the chemistry to find the sweet spot—stable enough to last in circulation, but still willing to hand over oxygen when your cells come calling.
Some of the most promising innovations come from unexpected sources. HemO2life, derived from a marine worm called Arenicola marina, has naturally polymerized hemoglobin that can transport up to 156 oxygen molecules per molecule—far exceeding what human hemoglobin achieves. This sea worm evolved to survive in oxygen-poor tidal mudflats, and scientists are now harnessing that evolutionary ingenuity for human medicine.
Perfluorocarbons sidestep the hemoglobin issues entirely. Because they physically dissolve oxygen rather than chemically binding it, they release oxygen smoothly based on concentration gradients. The downside is that you need to administer large volumes because PFCs carry less oxygen per unit volume than hemoglobin. They also require patients to breathe supplemental oxygen to maximize oxygen loading in the lungs.

The path from promising laboratory results to approved medical product is littered with failures and hard-won lessons. HemAssist became the first HBOC to receive FDA approval for clinical trials in the 1990s, using cross-linked hemoglobin from expired donated blood. Initial results looked encouraging, but Phase III trials revealed that patients receiving HemAssist faced increased risks of heart attacks and inflammation of the pancreas. The product was discontinued in 1999.
Other early HBOCs met similar fates. Researchers discovered that manufacturing these products at scale presented extraordinary challenges. Each deciliter of final product requires about 13 grams of purified hemoglobin protein—a massive amount of biological material that must be processed while maintaining absolute purity. Even trace amounts of endotoxins, bacterial contaminants that can trigger severe immune reactions, proved catastrophic. At contamination levels as low as 0.5 endotoxin units per milliliter, a single transfusion unit could deliver enough endotoxin to cause septic shock.
Despite these setbacks, some products have pushed through. Hemopure, made from cross-linked bovine hemoglobin, completed Phase III trials showing it could improve coronary oxygenation during cardiac surgery without significantly increasing mortality rates. The FDA granted expanded use approval, and Hemopure has been used in thousands of procedures. In animal studies, it even managed to restore brain circulation and function up to four hours after the heart had stopped—a result that could revolutionize emergency resuscitation if it translates to humans.
On the PFC front, Perftoran has seen real-world use in Russia, Kazakhstan, Ukraine, Kyrgyzstan, and Mexico, where over 35,000 patients have been treated. Two second-generation PFC products are currently in Phase III trials, benefiting from decades of refinement in oxygen capacity and emulsion stability.
Getting synthetic blood approved for widespread use involves navigating a regulatory gauntlet that makes pharmaceutical approval look simple. The FDA and equivalent agencies worldwide must be convinced that these products are not just effective but safer than the alternatives—including doing nothing and letting patients die from blood loss.
That's a high bar when your comparison point is a natural substance the human body has evolved to handle. Past clinical trials ended because patients experienced increased death rates and cardiovascular complications. Regulators understandably grew cautious, and the field entered a period of slow, methodical progress focused on understanding exactly what went wrong.
Manufacturing consistency represents another regulatory nightmare. When Oxylobin and Hemopure initially showed breakthrough results, some companies lost the institutional knowledge needed to reproduce those successes as leadership changed and key scientists moved on. New manufacturing platforms using single-use technologies promise endotoxin-free, scalable production with unprecedented safety profiles, but proving that consistency across batches takes time and rigorous testing.
Ethical debates swirl around resource allocation and access. If synthetic blood becomes available, who gets it first? Military applications have driven significant investment—synthetic blood doesn't require refrigeration, has a long shelf life, and works universally regardless of blood type. Those properties make it ideal for battlefield medicine. But should soldiers get priority over civilian trauma victims? And once approved, will synthetic blood remain a luxury for wealthy nations while developing countries continue struggling with contaminated donor blood?
Patent protections and pricing strategies add another layer of complexity. Companies that have invested hundreds of millions in research and development will seek returns that could price synthetic blood out of reach for the hospitals and regions that need it most. Public health advocates argue for compulsory licensing and technology transfer to ensure global access, while biotech executives counter that without intellectual property protection, the innovation pipeline will dry up.
Market analysts project the synthetic blood substitutes sector will explode from $9.73 billion in 2024 to $46.37 billion by 2034, representing a compound annual growth rate of 16.9%. Those numbers reflect not just the product sales but the broader economic impact of eliminating blood shortages.
Consider the costs avoided. Blood collection, testing, storage, and distribution form a complex and expensive infrastructure. Donated blood has a shelf life of about 42 days for red blood cells—shorter for platelets and other components. Significant quantities expire before use, representing pure waste. Hospitals maintain safety stocks that tie up refrigerated storage space and require constant monitoring.
Synthetic blood could eliminate much of that overhead. Room-temperature storage, extended shelf life, and universal compatibility mean hospitals could stock a single product instead of maintaining inventories of multiple blood types. Emergency response teams could carry synthetic blood to accident scenes, beginning treatment before patients even reach a hospital. Remote surgical facilities could perform complex procedures without worrying about blood supply.
The flip side is disruption to the existing blood donation ecosystem. Organizations like the American Red Cross and regional blood banks employ thousands of people and depend on government support and donor goodwill. A sudden shift to synthetic alternatives could destabilize that system before replacement infrastructure is ready. Some experts advocate for a gradual transition where synthetic blood supplements rather than replaces donation, preserving the social infrastructure around voluntary blood donation while addressing shortage gaps.
Insurance coverage will shape adoption patterns dramatically. If synthetic blood gets classified as an experimental therapy, patients could face crushing out-of-pocket costs. If it becomes standard of care, insurers must decide whether to pay premium prices for a product that could reduce complications and shorten hospital stays—potentially saving money in the long run.
North America currently dominates the market, driven by substantial R&D investment, advanced healthcare infrastructure, and government-funded programs for military and emergency medical applications. But Asia-Pacific regions are catching up quickly, with Japan and China investing heavily in domestic synthetic blood development. This geographic competition could accelerate innovation while raising questions about quality standards and international regulatory harmonization.

Emergency medicine stands to benefit most immediately. Trauma surgeons describe the "golden hour" after severe injury—the critical window when rapid treatment dramatically improves survival odds. Every minute spent on blood typing and cross-matching is a minute of oxygen deprivation for vital organs. Universal synthetic blood eliminates that delay entirely.
Imagine a car accident in rural Montana, hours from the nearest hospital. Paramedics arrive, establish IV access, and begin transfusing synthetic oxygen carriers within minutes. The patient's oxygen-starved brain and heart get relief long before reaching an operating room. Early animal studies suggest this approach could extend the window for successful resuscitation, potentially saving thousands of lives annually.
Military applications extend beyond combat medicine. Special operations forces deploying to remote locations could carry lightweight, shelf-stable synthetic blood instead of bulky refrigerated blood products. Submarine crews, aircraft carriers, and forward operating bases could maintain adequate supplies without the logistical headaches of blood collection and storage in austere environments.
Surgical teams might use synthetic blood to prime bypass machines for cardiac surgery, reducing the need for donated blood during complex procedures. Cancer patients undergoing intensive chemotherapy could receive synthetic oxygen carriers to manage anemia without depleting already-limited donated blood supplies. Jehovah's Witnesses and others who refuse donor blood for religious reasons would have a medically viable alternative.
Disaster response could be revolutionized. When hurricanes, earthquakes, or terrorist attacks overwhelm local blood banks, current protocols involve flying in supplies from other regions—a process that takes hours or days. Stockpiled synthetic blood could be deployed immediately, stabilizing mass casualties while donor recruitment ramps up.
One startup, working with university researchers, is developing biosynthetic blood that could eventually replicate more functions than just oxygen transport. Their approach combines engineered hemoglobin with synthetic cell membranes that mimic red blood cell properties. If successful, this could bridge the gap between simple oxygen carriers and true artificial blood capable of multiple functions.
Predicting exactly when synthetic blood will become standard in emergency rooms requires acknowledging uncertainty. Current Phase III trials for second-generation products suggest we're three to seven years from potential FDA approval for specific indications. Broader approval for general use could take a decade or more.
The path forward isn't just technological—it's cultural. Blood donation carries deep symbolic and social meaning. People donate blood to feel connected to their community, to honor loved ones, to give back. Surveys show Americans value plasma-derived medicines but may not fully understand where they come from. Building public acceptance of synthetic alternatives will require careful communication about safety, efficacy, and the continued importance of donation for blood components that can't yet be synthesized.
Regulatory agencies are adapting their frameworks to evaluate these novel therapies appropriately. The FDA has created specific guidance for oxygen therapeutics, recognizing that synthetic blood substitutes occupy a unique category. International coordination through organizations like the World Health Organization could help establish global standards and facilitate access in developing nations.
Research continues on third-generation products that address the limitations of current HBOCs and PFCs. Scientists are engineering hemoglobin variants with optimized oxygen binding curves, developing nanoparticle carriers that better protect hemoglobin from breakdown, and exploring entirely synthetic molecules that transport oxygen without any biological components. These advances could deliver products with safety profiles approaching or exceeding natural blood.
The synthetic blood story illustrates a broader pattern in medical technology—initial enthusiasm, sobering setbacks, patient refinement, and eventual transformation of clinical practice. Anesthesia, antibiotics, and organ transplantation all followed similar trajectories. Each faced skepticism, regulatory hurdles, and ethical debates before becoming standard care.
As synthetic oxygen carriers edge closer to widespread adoption, healthcare systems need to prepare for integration. Training protocols for emergency responders and surgical teams must evolve. Hospital formularies will need to make room for new products. Insurance policies will require updating to cover appropriate uses. Supply chains will shift from just-in-time blood delivery to stocking synthetic alternatives.
The ultimate success of synthetic blood won't be measured just in lives saved, though that matters most. It will show up in reduced healthcare costs, improved surgical outcomes, greater equity in access to emergency care, and enhanced resilience when disasters strike. It will free patients from dependence on the generosity of strangers and the limitations of biology.
We're not abandoning donated blood—we're supplementing it with a technology that could make blood shortages as obsolete as iron lungs and smallpox. The global blood shortage crisis may not last much longer. And when it ends, emergency medicine will never be the same.

Recent breakthroughs in fusion technology—including 351,000-gauss magnetic fields, AI-driven plasma diagnostics, and net energy gain at the National Ignition Facility—are transforming fusion propulsion from science fiction to engineering frontier. Scientists now have a realistic pathway to accelerate spacecraft to 10% of light speed, enabling a 43-year journey to Alpha Centauri. While challenges remain in miniaturization, neutron management, and sustained operation, the physics barriers have ...

Epigenetic clocks measure DNA methylation patterns to calculate biological age, which predicts disease risk up to 30 years before symptoms appear. Landmark studies show that accelerated epigenetic aging forecasts cardiovascular disease, diabetes, and neurodegeneration with remarkable accuracy. Lifestyle interventions—Mediterranean diet, structured exercise, quality sleep, stress management—can measurably reverse biological aging, reducing epigenetic age by 1-2 years within months. Commercial ...

Data centers consumed 415 terawatt-hours of electricity in 2024 and will nearly double that by 2030, driven by AI's insatiable energy appetite. Despite tech giants' renewable pledges, actual emissions are up to 662% higher than reported due to accounting loopholes. A digital pollution tax—similar to Europe's carbon border tariff—could finally force the industry to invest in efficiency technologies like liquid cooling, waste heat recovery, and time-matched renewable power, transforming volunta...

Humans are hardwired to see invisible agents—gods, ghosts, conspiracies—thanks to the Hyperactive Agency Detection Device (HADD), an evolutionary survival mechanism that favored false alarms over fatal misses. This cognitive bias, rooted in brain regions like the temporoparietal junction and medial prefrontal cortex, generates religious beliefs, animistic worldviews, and conspiracy theories across all cultures. Understanding HADD doesn't eliminate belief, but it helps us recognize when our pa...

The bombardier beetle has perfected a chemical defense system that human engineers are still trying to replicate: a two-chamber micro-combustion engine that mixes hydroquinone and hydrogen peroxide to create explosive 100°C sprays at up to 500 pulses per second, aimed with 270-degree precision. This tiny insect's biochemical marvel is inspiring revolutionary technologies in aerospace propulsion, pharmaceutical delivery, and fire suppression. By 2030, beetle-inspired systems could position sat...

The U.S. faces a catastrophic care worker shortage driven by poverty-level wages, overwhelming burnout, and systemic undervaluation. With 99% of nursing homes hiring and 9.7 million openings projected by 2034, the crisis threatens patient safety, family stability, and economic productivity. Evidence-based solutions—wage reforms, streamlined training, technology integration, and policy enforcement—exist and work, but require sustained political will and cultural recognition that caregiving is ...

Every major AI model was trained on copyrighted text scraped without permission, triggering billion-dollar lawsuits and forcing a reckoning between innovation and creator rights. The future depends on finding balance between transformative AI development and fair compensation for the people whose work fuels it.